Katherine Connor, UC San Diego

This story is from the 2025 issue of Discoveries, a UC San Diego Health Sciences magazine.
For the past five years, several University of California San Diego electrical engineering graduate students have spent one day a week at the Joan and Irwin Jacobs Retina Center at Shiley Eye Institute. Jacobs Retina Center is the only freestanding retina research center in the country, working to increase the understanding of retinal diseases, such as macular degeneration and diabetes-related blindness, and to conduct clinical trials to develop better treatments for these diseases. But the students aren’t there for treatment, and they’re not there to see patients.
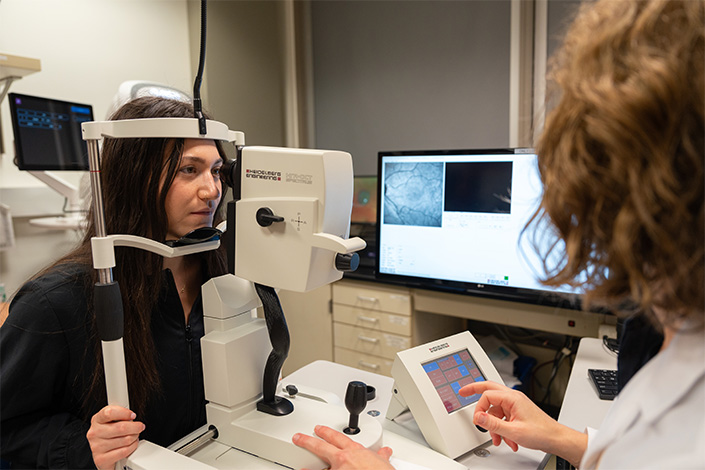
Neurobiology student Sarah Shacterman volunteers to have her retina scanned.
Through a unique and long-standing collaboration, the electrical engineers are embedded in Jacobs Retina Center to partner with ophthalmologists to: develop better computer vision, artificial intelligence (AI) and image processing tools to help physicians diagnose patients faster and more accurately; predict which drugs will be most successful for specific patients; and even aid in the process of developing new therapeutic treatments for retinal diseases.
Over the course of five years, the engineers and ophthalmologists have collaborated on 21 papers, publishing advances in both clinical and engineering journals.
“We started out with the questions of whether we could help ophthalmologists align images of the retina and whether AI can actually help doctors be faster and more accurate with their detection of disease,” said Troung Nguyen, professor of electrical and computer engineering at the Jacobs School of Engineering at UC San Diego. “And we have done that. In this collaboration, it has been very critical to have both the expertise on the engineering side, with machine learning, image processing and so on, and the expertise from the clinical side. We have been very successful in terms of getting results and have made a big, broad impact.”
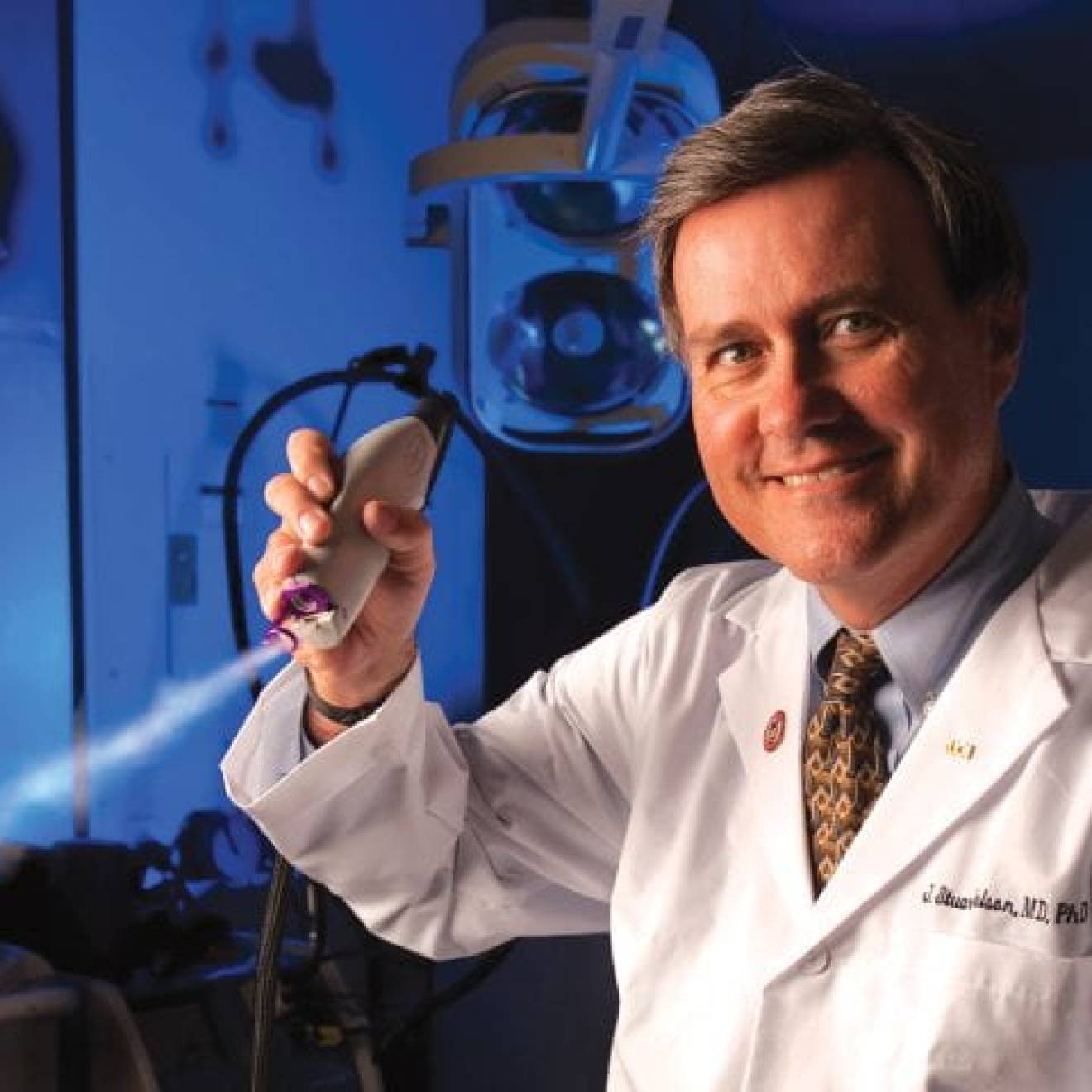
The graduate students in Nguyen’s lab partnered with William Freeman, M.D., Distinguished Professor and vice chair of the Viterbi Family Department of Ophthalmology at UC San Diego School of Medicine and director of Jacobs Retina Center at Shiley Eye Institute. Freeman and Nguyen add that such a longstanding and impactful partnership, benefitting both fields of research, is extremely unique.
“It’s exceptionally rare to have weekly discussions where engineers actively engage with patient care, making it easier to understand their work and needs,” said Freeman. “Our collaborations aren’t just one-offs; even after someone may work with us for two to three years and earns their Ph.D., the ongoing connection is unique. This sustained effort, bridging medicine and engineering across campus, isn’t just about claiming that we use AI — it’s a dedicated approach to tackling practical health care challenges through innovation.”
A speedier diagnosis
While this collaboration has yielded nearly two dozen scientific publications to date, with more in the pipeline, there are several particularly noteworthy examples of this collaborative research leading to better outcomes for patients. Most recently, the joint team developed an AI tool that was able to predict whether a patient had age-related macular degeneration just by looking at optical coherence tomography (OCT) angiography images of a patient’s blood vessels in their eye. These images are noninvasive and taken in several minutes during a standard clinical visit. The AI tool allows ophthalmologists to glean the same information from photos that they would previously have needed to perform a biopsy to assess. And it outperformed human experts with 80% accuracy based on images alone.
Not only was the tool able to help doctors diagnose patients faster and more accurately, but it could also be used to develop better drugs to treat macular degeneration.
In another paper, the team devised a way to synthesize multiple images from different time points to more accurately check if there has been growth in the size of blood vessel damage or a tumor, for example.
“When you’re looking at retinal diseases in the retinal periphery, or the outer edges, they are difficult to see,” said Freeman. “To track changes over time, typically, you would compare images from the previous and current years to see if it has grown past a specific point, like a blood vessel or marker.”
The engineers developed a method to overlap previous images with the current image of a patient’s eye so that it’s immediately evident whether the object in question has grown or changed from previous years. The AI method localized the spot in question 37 percent faster than the traditional side-by-side image comparison, and with a 0 percent error rate, compared to 18 percent error rate in a side-by-side comparison by ophthalmologists.
The ophthalmologists and engineers have developed deep learning networks to correct eye motion in 3D retinal imaging, quantitatively evaluate morphological changes in vasculature due to age-related macular degeneration using OCTA angiography, corrected distortions between ultra-widefield and narrow-angle retinal images, and created an AI tool to overlay multimodal images from different optical instruments in patients with retinitis pigmentosa, among many other joint advances.
The clinicians are adamant that these algorithms and models are ultimately just tools and are meant to enhance, not replace, the expertise and ethical decision-making of ophthalmologists.
Engineering for the public good
Bo Wen, an electrical engineering graduate student who is collaborating on these ophthalmology projects, said having such tangible results has been a huge motivator for him and the other electrical engineering students involved.
“If we’re not actually helping people, then why are we doing this?” Wen said. “If we are only here to get some papers published, that’s too superficial. We want to have our work make an impact in disease diagnosis and treatment.”
Nguyen encouraged other faculty and students at UC San Diego to invest the time to develop collaborations across campus. With nearly 4,000 faculty members working on leading-edge research, there are endless opportunities to apply expertise in a new way.
“The real power of this collaboration is that we understand our expertise, we understand our contributions, and we regularly meet with one another to see how we can both leverage that expertise,” said Nguyen. “There are many opportunities for engineers to branch out and really serve and make an impact on real problems — that’s what I love the most about this.”