Andy Fell, UC Davis

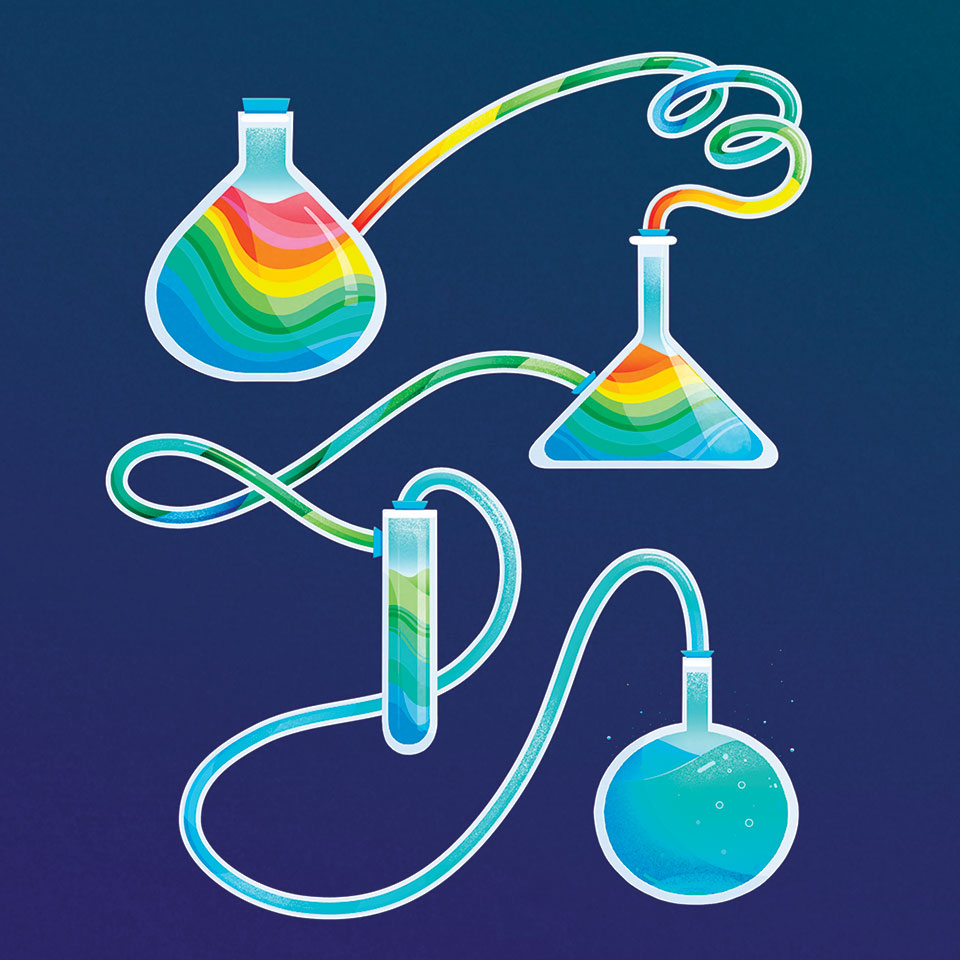
UC Davis researchers are bringing the benefits of drugs like LSD and cannabis to light. They may be the next big thing in pharmaceuticals for treating a range of problems like depression and anxiety.
For decades, possession and use of drugs like LSD and cannabis has come with a threat of prosecution and jail time. But in the past few years, researchers have started taking a closer look at these compounds, finding potential for new treatments for psychiatric and central nervous system problems such as seizures, depression, anxiety and post-traumatic stress disorder. UC Davis scientists are among the small group of licensed researchers pushing the field forward — including launching startup companies to help bring these new drugs to market.
The need for new drugs
Mental health disorders are very common. About 1 in 5 Americans live with some form of mental illness, according to the National Institute of Mental Health.
Drugs are available to help these patients, said Cameron Carter, distinguished professor in the UC Davis Department of Psychiatry and Behavioral Sciences, and Center for Neuroscience. “We have a repertoire of effective treatments that we didn’t have 30 or 40 years ago.”
At the same time, existing drugs have drawbacks, Carter said. They are slow-acting, taking days or weeks to show effect. Not all patients respond to current treatments, and they are based on a limited understanding of the root causes of mental illness.
UC Davis associate professor in chemistry David Olson became interested in psychedelic drugs for psychiatric treatment as a postdoctoral researcher at the Broad Institute in Cambridge, Massachusetts.
At the time, a lot of research focused on ketamine, Olson said. Ketamine is used as an anesthetic and also abused as a recreational drug. But it also turns out to be a remarkably effective antidepressant. Ketamine acts within hours, and the effect of a single treatment can last for up to a week, Olson said. It works across a range of indications including depression, PTSD and substance abuse.
In 2019, the U.S. Food and Drug Administration approved esketamine, a version of the drug delivered as a nasal spray, for treatment of severe, treatment-resistant depression. The treatment has to be given in a clinical setting, where the patient is monitored for several hours.
A common feature of disorders such as depression, anxiety and PTSD is atrophy, or withering of neurons in the prefrontal cortex. Ketamine appears to act by reversing this atrophy and repairing neural connections in the brain.
Olson wondered if there might be other molecules with a similar effect and started to look at psychedelics such as LSD, MDMA and DMT (the active component in the herbal drug ayahuasca).
Olson joined the UC Davis faculty in 2015, and in 2018, his group published papers showing that a wide variety of psychedelics could cause nerve cells to form new connections and that they could help rodents overcome “fear responses” — a model for anxiety and PTSD.
Olson named this class of drugs “psychoplastogens” because they encourage neural plasticity, or the regrowth of structures that make connections between neurons.
A healing-based approach
Recently published results show that MDMA and psilocybin, in combination with psychotherapy, are effective in treating PTSD and depression. Olson said that one or more of these drugs — still widely illegal — could soon be approved for clinical use.
But major barriers to psychedelics in clinical use still exist. The possibility of hallucinogenic side effects, and the stigma of illegality, could put off both physicians and patients. More significantly, psychedelic therapy is usually accompanied by psychotherapy before and after drug treatment, and the patient needs to be monitored during their trip. That makes treatment expensive compared to a daily or weekly pill you can keep in the bathroom cabinet.
“Scalability is a huge issue for psychedelics,” Olson said. “A big goal of mine is to produce medicines that are accessible to everyone.”
Olson’s laboratory aims to separate the ability to repair damaged neural connections in the brain from the psychedelic properties of these drugs. The goal is a drug that is fast-acting with a lasting effect from a single dose and does not cause side effects such as hallucinations.
To achieve this, they take the chemical structures of known psychedelic drugs and alter them to come up with new candidates that can be tested for their psychoplastogenic properties in cell cultures and animal models.
Ibogaine, for example, is a psychedelic drug extracted from the iboga tree, Tabernanthe iboga. Ibogaine is reputed to be effective in treating addiction, but it also causes hallucinations and heart problems.
Olson’s laboratory synthesized a number of compounds similar in structure to ibogaine and came up with one they called tabernanthalog, or TBG. Similar to other psychoplastogens like ketamine, LSD and MDMA, tabernanthalog promoted growth of branches and spines in rat nerve cells, and showed positive effects in animal models of depression and addiction. It did not have negative effects on the heart like ibogaine, and it did not cause a “head twitch” response in mice, considered to be a marker for hallucinations in humans. The work was published in Nature in 2021.
In 2019, Olson founded a startup company, Delix Therapeutics Inc., to help develop these promising drug candidates and bring them to market. So far, Delix has raised about $100 million in funding and plans to bring two compounds into phase 1 clinical trials sometime this year.
“I’m so excited about this class of molecules,” Olson said. While currently approved drugs treat the symptoms of mental illness, Olson believes that psychoplastogens have the potential to restore the prefrontal cortex, a key region of the brain involved in motivation, cognition and decision-making in the human brain.
“It’s a paradigm shift to a healing-based approach,” he said.
Speeding drug development
One problem with developing new drugs based on psychedelics is how to screen out those that cause hallucinations before they get to human trials. The rodent head twitch test is considered to be a reliable predictor, but you can’t really ask a mouse if it’s hallucinating. This presents a bottleneck for developing new drugs.
“We don’t have good ways to screen neurological drugs at scale,” said Lin Tian, professor of biochemistry and molecular medicine in the UC Davis School of Medicine. Tests that could be carried out in cell culture would allow for more rapid screening.
Tian’s lab uses light-based technology to study the chemical messengers and receptors that carry signals in the brain. After Olson gave a departmental seminar on drugs affecting the serotonin 2A receptor, the two laboratories began collaborating.
Graduate students Jason Dong, Calvin Ly and Lee Dunlap came up with psychLight, a modified version of the serotonin 2A, or 5-HT2A, receptor with a fluorescent tag. When psychLight is engaged by a hallucinogenic drug it changes shape slightly, causing its fluorescence to increase. Nonhallucinogenic compounds binding to psychLight cause a different fluorescence profile.
PsychLight can be used to rapidly screen large numbers of candidate molecules for potential to cause hallucinations, in biochemical assays or in cell cultures. This approach can also be used to carry out basic research on brain signaling, which is fundamental for understanding the basis of psychiatric diseases, Tian said.
“I’m very excited about how both drug discovery and basic science can be pushed forward by this technology,” she said.
Tian and former graduate student Grace Mizuno have also founded a company, Seven Biosciences, which has an exclusive license from UC Davis on psychLight and related technology. Their goal is to speed up drug discovery by creating a platform that pharmaceutical companies can use to rapidly screen compounds for neurological effects.
Cannabis coming up green
While Olson is working on analogs of psychedelic drugs, fellow chemistry professor Mark Mascal is working on analogs of cannabidiol, or CBD, one of the active components in cannabis.
Cannabis, like the psychedelic drugs, is a Schedule 1 controlled substance under federal law, although its production, possession and use is legal under state law in California and a few other states. CBD derived from the closely related hemp plant is legal under federal law if certain conditions are met.
One formulation of CBD, sold as epidiolex, is approved by the FDA as a prescription treatment for severe seizures. CBD also has potential for treating metabolic syndrome, cognitive decline and in muscle recovery from injury, Mascal said.
Some people buy over-the-counter CBD from dispensaries to manage conditions such as anxiety. But the potency of retail CBD products isn’t high enough to have therapeutic effects, Mascal said. “It’s probably a placebo effect,” he added.
Legality is still an important aspect of developing CBD as a drug, including internationally, Mascal said. It is relatively simple to convert CBD to tetrahydrocannabinol, or THC, which gives cannabis its psychoactive properties. That raises concern that legalized CBD products could be diverted to produce recreational THC.
Instead, Mascal’s lab works with 8,9-dihydrocannabidiol or H2CBD, a synthetic analog of the drug, which cannot be converted to THC. They developed a method to synthesize H2CBD and showed that it could successfully treat seizures in rats. That work was published in 2019 in Scientific Reports.
Mascal has founded a startup company, Syncanica, to develop similar compounds that he calls pseudocannabinoids. These are not, he said, “synthetic cannabis” but entirely different compounds. Mascal hopes to win investigational new drug status for H2CBD from the FDA this year so that the drug can enter clinical trials.
A new center for research
In 2019, UC Davis established the Cannabis and Hemp Research Center as a special program under the Office of Research. Co-directors of the center are Carter and Li Tian, professor of plant sciences in the College of Agricultural and Environmental Sciences. The center facilitates collaborations and supports research related to cannabis and hemp. Research topics range from cultivation and production, the economics of the industry, to experimental research on cannabis derivatives and clinical trials.
Among other projects at the center:
-
Postdoctoral researcher Karen Wagner and Professor Bruce Hammock, from the Department of Entomology and Nematology, are investigating CBD’s potential as a pain medication.
-
Mascal and Michael Rogawski, distinguished professor of neurology, are working on Mascal’s H2CBD as a retreatment for various forms of epilepsy.
-
Professor Keith Baar, Department of Membrane Biology and Physiology, and researcher Henning Langer are leading a study of the effects of CBD and H2CBD in treating congenital muscular dystrophy.
-
Professor Melissa Bauman, Department of Psychiatry and Behavioral Sciences, is studying the effects of prenatal exposure to THC on brain development.
-
Tyler Lesh, a clinical psychologist in Carter’s lab, is conducting a study of the relationship between cannabis use and psychosis. The work is funded by the California Bureau of Cannabis Control.
Heavy cannabis use is known to be associated with increased risk of psychosis, Lesh said. The risk is highest in childhood and adolescence and is increased in people with a family history of psychosis. But the effects can be positive, including lower blood pressure, better metabolic profile and reduced abdominal girth.
“We’re trying to get a more nuanced picture of how cannabis use impacts people with psychosis,” Lesh said. The study, which began in December 2021, includes volunteers from the community with any degree of psychosis. Subjects get a thorough workup including metabolic profiles, body mass index, questions on activity levels, diet and symptoms, and brain scans.
Using psychedelics to understand the brain
Much of the current research on psychedelic drugs is empirical — taking existing drugs (LSD, MDMA, ibogaine) and testing them against conditions like depression, anxiety and PTSD in patients.
“There’s growing evidence that these drugs work well and work quickly in patients resistant to other treatments,” Carter said.
Yet we still have a very limited understanding of how the brain works and of the causes of these illnesses. Addressing this gap in basic knowledge is the goal of the proposed UC Davis Center for Psychedelics and Neurotherapeutics. To be led by Olson and John Gray, associate professor in the Department of Neurology, and Center for Neuroscience, the center would draw on UC Davis’ unique combination of programs and strengths, including the schools of Medicine and Veterinary Medicine, College of Letters and Science, College of Biological Sciences, California National Primate Research Center and Mouse Biology Program, Neuroscience Consortium, Center for Mind and Brain, Imaging Center and many others.
Modern neuroscience is highly collaborative, Olson said, but working with drugs classed as Schedule 1 by the Drug Enforcement Agency requires a special license. That makes collaboration between universities even harder if the other institution doesn’t have a Schedule 1 license. But the breadth of expertise and facilities available within UC Davis means collaboration within the campus is quite feasible.
“UC Davis is unique because we can do most everything in-house,” Olson said. The center would bring together researchers interested in neurotherapeutics, offering pilot grants for basic research.
The research at UC Davis has the potential to help many patients, Carter said.
“It’s opening a whole new range of approaches, which should offer hope to people with treatment-refractory mental health problems and their loved ones,” he said.
Glossary of drugs
Cannabidiol
Cannabidiol, or CBD, is extracted from cannabis and hemp plants. A formulation of CBD is approved for treating severe seizures. Potential medical uses: Treating seizures, metabolic syndrome, cognitive decline and in repairing damaged muscles
DMT
The psychedelic drug dimethyltryptamine, or DMT, is naturally occurring in a number of plants and animals and has a rapid onset. Potential medical uses: Treatment-refractory depression
Ibogaine
A psychedelic drug extracted from the iboga tree, Tabernanthe iboga, it is currently legal by prescription in a few countries including Australia and Canada. Potential medical uses: Treatment-refractory depression, anxiety, PTSD and substance abuse
Ketamine
Originally an anesthetic, it is approved by the FDA for general anesthesia. A nasal spray version is approved for treating severe depression. Potential medical uses: Treatment-refractory depression, PTSD, substance abuse
LSD
Lysergic acid diethylamide, or LSD, is more potent and longer lasting than some of the other psychedelic drugs. Potential medical uses: Treatment-refractory PTSD, anxiety, depression and substance abuse
MDMA
Methylenedioxymethamphetamine, or MDMA, is commonly known as ecstasy and molly, and was used in psychotherapy before it was widely banned. Potential medical uses: Treatment-refractory PTSD, anxiety and depression
Psilocybin
Produced in more than 180 species of mushrooms, this compound has a similar structure to LSD. Potential medical uses: Treatment-refractory PTSD, anxiety and depression