Suzanne Leigh, UC San Francisco
Traumatic brain injury (TBI) results in close to 70,000 deaths in the U.S. every year, and it is the cause of long-term physical, cognitive and mental disability in 5 million Americans. But despite three decades of work, treatments are sorely lacking.
Now, an innovative drug development trial will be available in emergency departments of 18 level 1 trauma sites nationwide. It is being launched by UC San Francisco and the Transforming Research and Clinical Knowledge in Traumatic Brain Injury Network (TRACK-TBI Network).
The study is made possible under an agreement with the Department of Defense, U.S. Army Medical Materiel Development Activity (USAMMDA), Fort Detrick, Md., which has supported research into TBI, particularly since the conflicts in Afghanistan and Iraq. More than 300,000 service members have sustained a TBI, typically caused by blasts and explosions, vehicle crashes and falls.
In the civilian population, TBI is most often caused by vehicle crashes and falls. Older adults, as well as those facing barriers in accessing appropriate care, are the fastest-growing population with TBI and are at higher risk of disability and death.
The clinical trial is enrolling participants who have conditions that range from moderate TBI to mild TBI, also known as concussion, to see if drugs that are already on the market for other disorders may be effective for TBI.
The first three drugs in the trial, which were developed to treat blood pressure, infection and high cholesterol, have shown promise for treatment of TBI in small studies.
"Adaptive platform" broadens opportunities for patients, researchers
“While most clinical trials test one treatment at a time, we are using an adaptive platform that allows us to test three drugs at the same time,” said principal investigator Geoffrey Manley, MD, PhD, professor of neurosurgery at UCSF and chief of neurosurgery at Zuckerberg San Francisco General Hospital. Manley also heads TRACK-TBI, a UCSF-led brain injury research initiative, which is screening participants and conducting follow-up testing.
“This means participants will have a 3 in 4 chance of receiving the drug rather than the placebo, compared to a 1 in 2 chance in a traditional trial,” Manley said. “It also means that we can add new therapies as the trial progresses and eliminate those that are not working.”
The study follows more than 30 clinical trials that have failed to show effectiveness. Manley said this is due in part to the absence of biomarkers that provide critical information about participants’ level of injury and potential for recovery.
Recent breakthroughs highlighted in TRACK-TBI studies in which Manley was the senior author are helping clinicians in the current trial to screen for appropriate participants and monitor their progress.
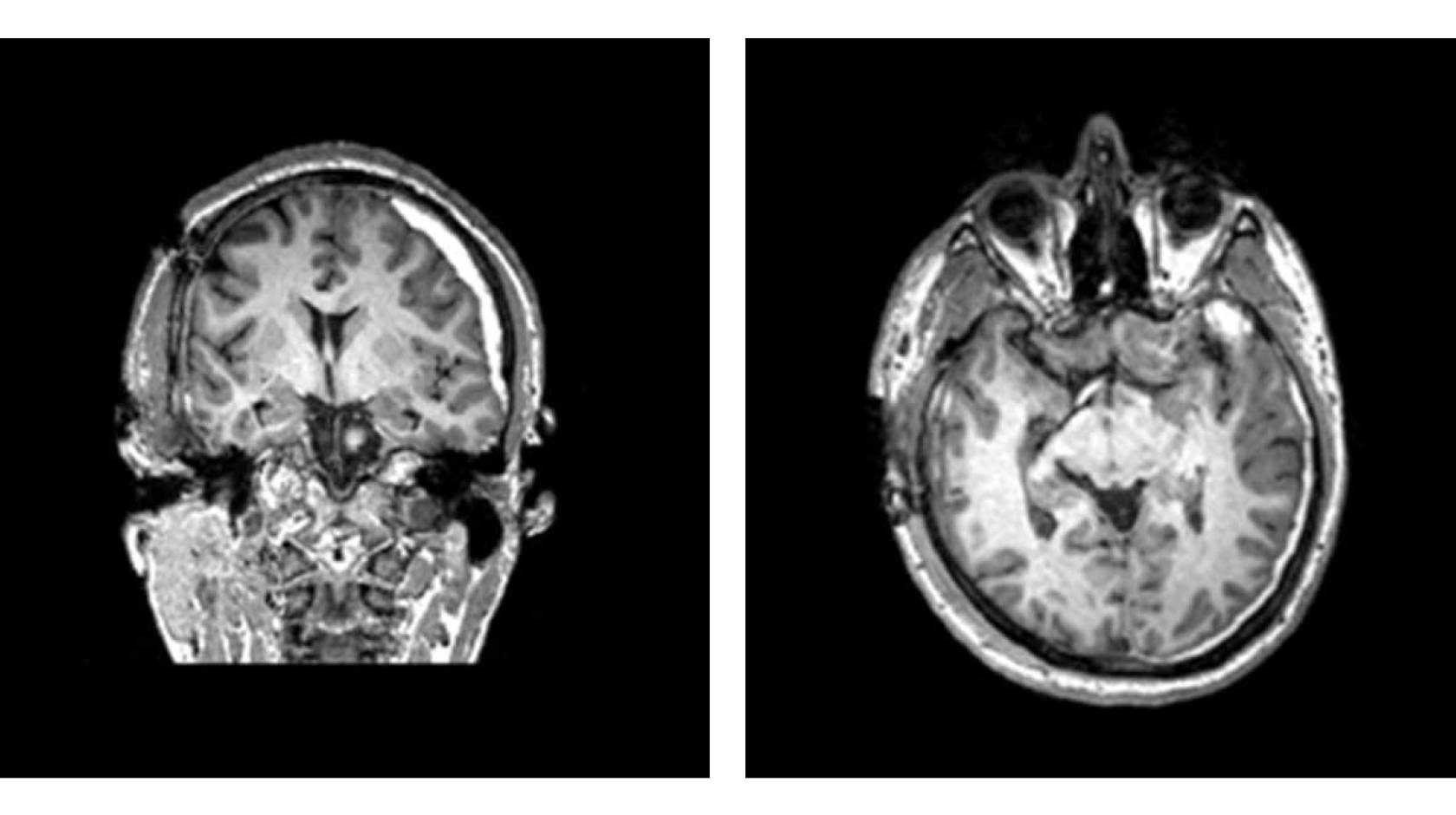
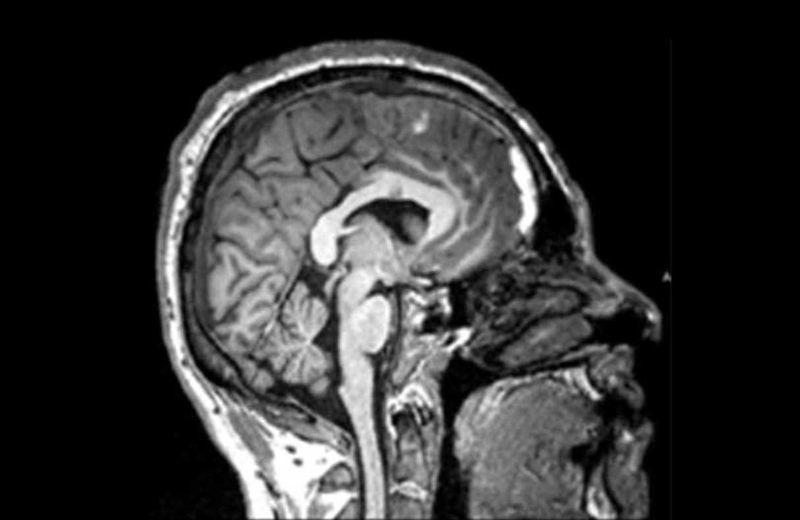
These include research showing that higher levels of two protein biomarkers identified in a newly injured patient’s blood indicate a TBI, despite a CT scan that appears normal. These biomarkers also flag the patients who are likely to die, and those who are likely to survive but with severe injuries. Conversely, lower levels of the biomarkers indicate an accident has not caused a brain injury.
Another study that could help identify patients for the current trial showed that patients with certain patterns of injury that are visible on their CT scans were less likely to make a complete recovery a year later.
Trial participants must enroll on the day of their injury, so they can be treated promptly. They must have a CT scan showing evidence of bleeding, and a blood test and exam that indicate moderate to mild TBI.
“We hope that this trial will lead to effective treatments and future collaborations with pharmaceutical companies,” said Manley, who is a member of the UCSF Weill Institute for Neurosciences.
“One of the barriers in treatment development has been a relative absence of public awareness about TBI. It’s an area that lacks patient-led advocacy,” he said. “TBIs occur suddenly, without warning, leaving families and patients in no position to champion the cause.”
The first four participants of the trial were enrolled at UCSF in August. Other TRACK-TBI Network sites are preparing to accept participants in the coming months. The trial will enroll a total of 672 participants over the next four years.
About USAMMDA: The U.S. Army Medical Materiel Development Activity develops, delivers, and fields critical drugs, vaccines, biologics, devices, and medical support equipment to protect and preserve the lives of Warfighters across the globe. USAMMDA Project Managers guide the development of medical products for the U.S. Army Medical Department, other U.S. military services, the Joint Staff, the Defense Health Agency, and the U.S. Special Operations community. The process takes promising technology from the Department of Defense, industry, and academia to U.S. Forces, from the testing required for U.S. Food and Drug Administration approval or licensing to fielding and sustainment of the finished product. USAMMDA Project Management Offices will transition to a Program Executive Office under the Defense Health Agency, Deputy Assistant Director for Acquisition and Sustainment.
Traumatic brain injury results in close to 70,000 deaths in the U.S. every year, and it is the cause of long-term physical, cognitive and mental disability in 5 million Americans. But despite three decades of work, treatments are sorely lacking.

