Sonia Fernandez, UC Santa Barbara
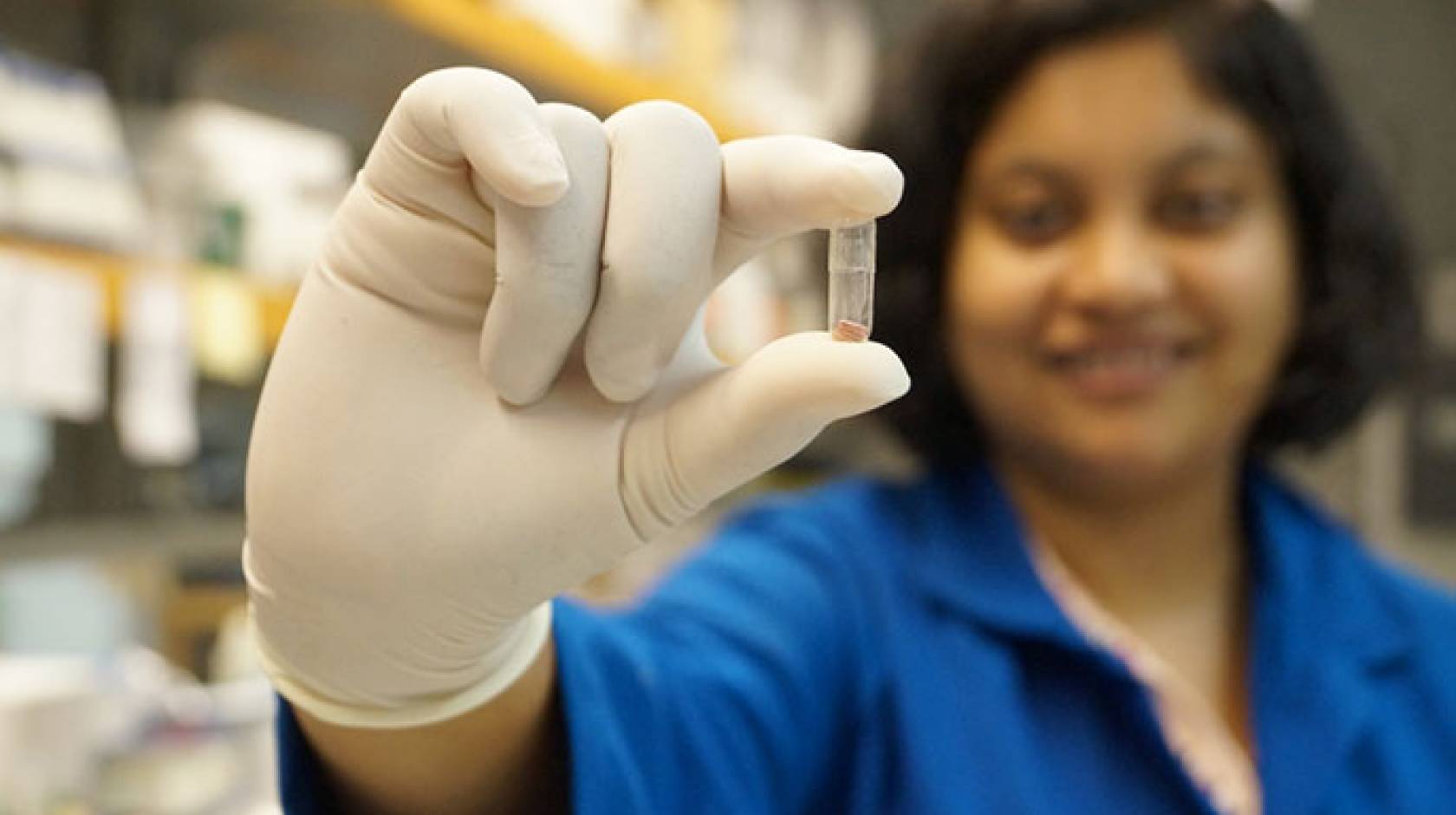
An insulin pill being developed by researchers at UC Santa Barbara may in the near future give another blood sugar management option to those who suffer from diabetes. The novel drug delivery technology may also apply to a wide spectrum of other therapies.
“With diabetes, there’s a tremendous need for oral delivery,” said Samir Mitragotri, a professor in the Department of Chemical Engineering who specializes in targeted drug delivery. “People take insulin several times a day and delivery by needles is a big challenge.”
According to the Centers for Disease Control’s 2014 estimates, more than 29 million individuals in the U.S. have undiagnosed or diagnosed diabetes. Many of these people would require regular insulin shots. For those who don’t like needles, the discomfort injections can pose is a huge barrier to compliance, said Amrita Banerjee, a postdoctoral researcher in the Mitragotri Lab. “It can lead to mismanagement of treatment and complications that lead to hospitalization,” she said.
A pill, said the researchers, could circumvent the discomfort associated with the needle while potentially providing a more effective dose.
“When you deliver insulin by injection, it goes first through the peripheral bloodstream and then to blood circulation in the liver,” Mitragotri explained. Oral delivery would take a more direct route, he added, and, from a physiological point of view, a better one.
Running the gauntlet
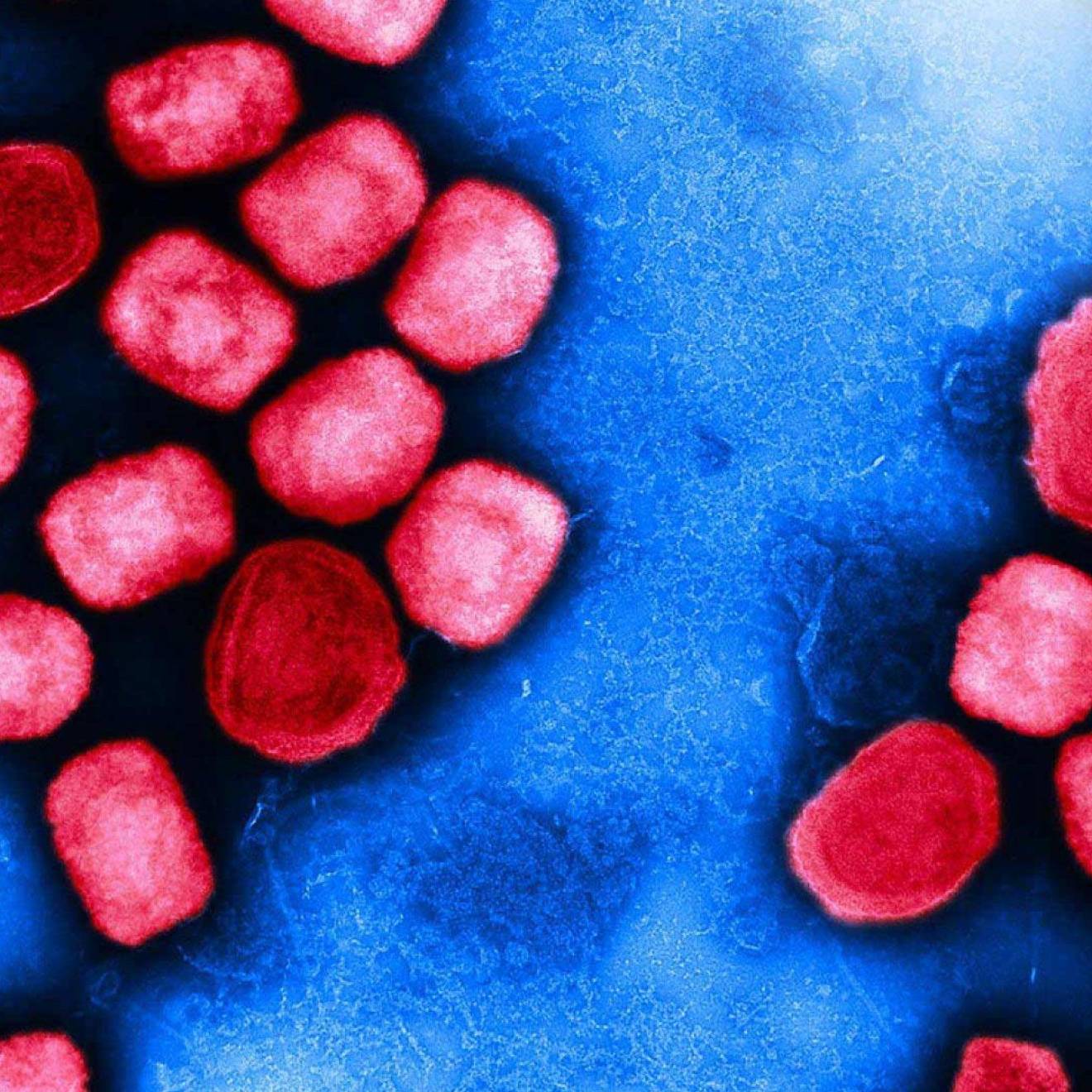
While oral medications to assist the body with insulin production have been around for a while, a pill that delivers insulin remains a highly sought goal of diabetes medicine. The main obstacle to its development has been getting the medication past the hostile proteolytic environment of the stomach and intestine without destroying the protein itself. In this case, the key is a combination of enteric-coated capsules and insulin-loaded mucoadhesive polymer patches that were optimized by Banerjee as part of her research. The new pill has demonstrated its ability to survive stomach acids with the protection of the enteric-coated capsule and deliver its payload to the small intestine. There, the capsule opens up to release the patches that adhere to the intestinal wall, preventing access of proteolytic enzymes to insulin and, with the aid of a permeation enhancer, depositing insulin that can pass through to the blood.
“This is the first essential step in showing that these patches can deliver insulin,” Mitragotri said. Like any other novel therapy, however, it must undergo additional stages of testing and improvement before it can be considered as a viable treatment for diabetes. Results of this research were presented in October at the American Association of Pharmaceutical Scientists’ annual meeting and exposition in Orlando, Florida.
Hope for the needle phobic
According to the researchers, the drug-loaded mucoadhesive patches show early promise for other forms of therapy, as well.
“We can deliver many proteins that are currently injected,” Mitragotri said. Other protein-based therapies such as growth hormones, antibodies and vaccines could potentially be put into patch form for painless delivery and improved patient compliance, he added.
Research for this project was funded by the National Institutes of Health (NIH # 1R01DK097379-01A).