Janet Wells, UCSF

Oliver Bishop has sandy blond hair styled like a 1940s screen idol’s and a scruffy beard and sideburns that frame his wide smile. A senior in high school, he is busy – singing with his school’s award-winning jazz choir, leading the marching band, teaching music lessons. Outgoing and popular, he was elected homecoming king in the fall.
Bishop, 18, was assigned female at birth and had spent years trying – and failing – to make peace with that status.
The disconnect he felt with his body didn’t matter so much when he was young, a tomboy in his hometown in California’s Sierra foothills. He refused to wear dresses, played on a coed baseball team, and ran around in swim trunks with no top.
Things changed abruptly in fourth grade, when he started puberty. He tried to fit in, growing his hair long and wearing more feminine clothes. He was increasingly miserable and unable to name what was wrong. His grades plummeted. He chopped off his hair.
“A buzz cut, that took a lot off me emotionally,” he says. But he still felt trapped in a body growing more feminine by the day. By the time he reached high school, his distress was at a crisis level. He thought about suicide.
A few months before his 15th birthday, Bishop stumbled across the word “transgender” online. He read about people who had had medical treatment to align their bodies with their gender identity – their inner sense of who they are.
“Bam, my life changed,” he says. “It lifted a major weight to find out I could do something about all this pressure I had been feeling.”
“I didn’t know how to fix it,” he says. “I didn’t have anything to strive for.”
Coming out to his parents, however, “was an ordeal.” He wrote a letter but never gave it to them. Finally, he blurted it out when his mother dropped him off at a friend’s house for the night. “Mom, I’m trans,” he said, jumping out of the car. His father stopped speaking to him for months.
“We live in a small, conservative place,” Bishop says. “The community I was raised in didn’t have any idea of what transgender was.”
His parents didn’t understand, says Bishop. But they loved him and knew he – and they – needed help. Their family doctor mentioned UCSF’s Child and Adolescent Gender Center. At their first appointment, both of his parents cried.
“I thought they were upset,” says Bishop. “But it was because they were so happy to see people who understood me.”
That visit, he adds, “changed everything.”
A shifting landscape
The conversation on gender identity has surged into the mainstream in recent years, with the emergence of celebrities like Caitlyn Jenner, the bestselling book Becoming Nicole, and the award-winning Amazon series Transparent.

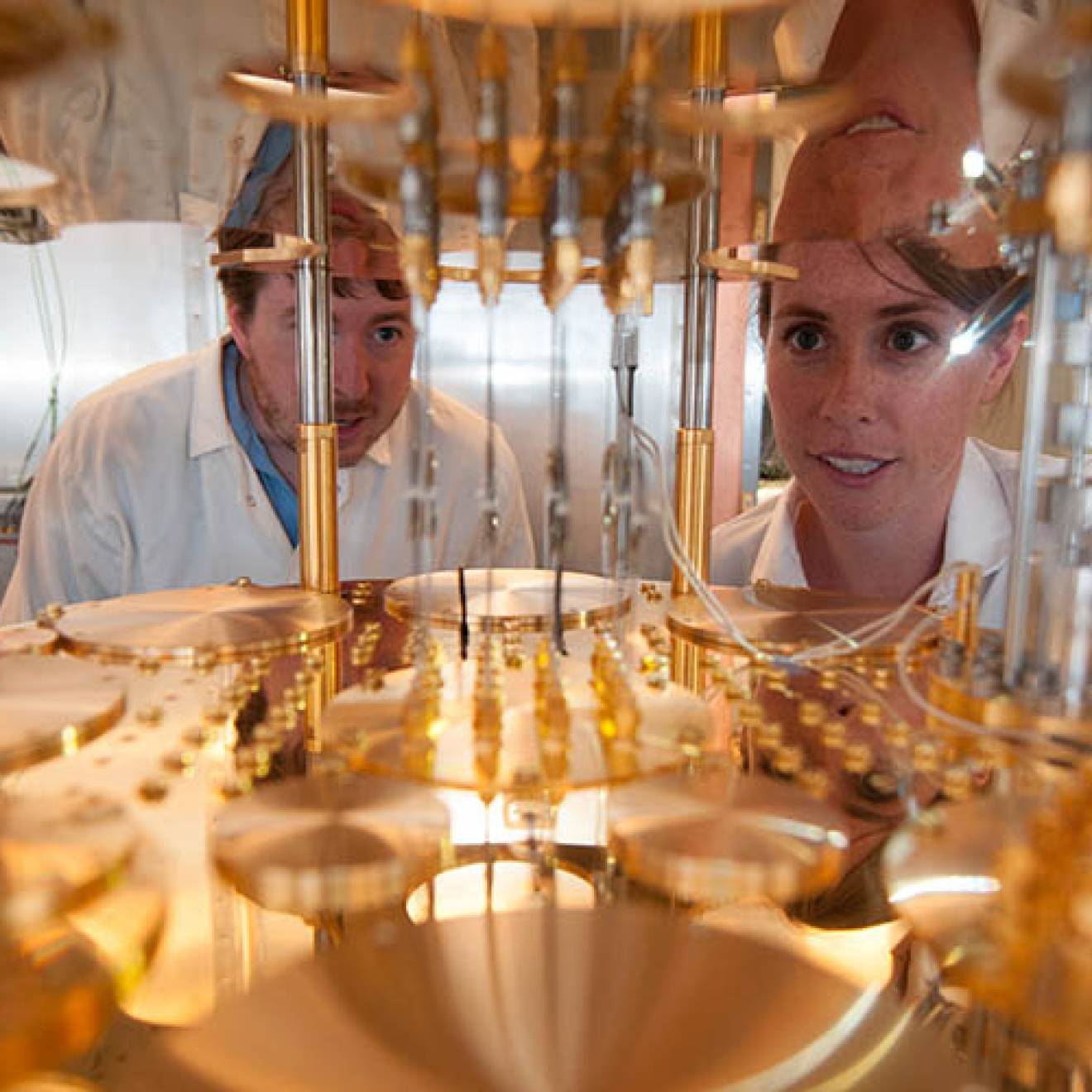
Credit: Stefan Hundhammer (top) and Audrey Feely/UCSF
Half of adults aged 18 to 34 now see gender as a spectrum from male to female, not as a binary assignment, according to a survey conducted last year by the website Fusion.net. The American Dialect Society’s 2015 Word of the Year was the singular pronoun “they” as an alternative to “he” or “she.”
The rapid shift in attitude is more than cultural. California recently mandated that public school students have access to bathrooms, locker rooms, and sports teams based on their gender identity, regardless of the gender on their records.
Significantly, in 2013, the Diagnostic and Statistical Manual of Mental Disorders – American psychiatry’s clinical bible – replaced “gender identity disorder” with “gender dysphoria.”
As a result, cross-gender identity in itself is no longer considered a mental illness, much as homosexuality was reclassified in the 1970s. The focus instead is on distress stemming from incongruence between the gender that individuals are assigned at birth, based on their physical characteristics, and their internal gender identity.
That distress can reach alarming levels: Transgender youth have a two- to threefold increase in risk of depression, anxiety disorder, suicidal ideation, and attempted suicide, according to a 2015 study in the Journal of Adolescent Health.
“Not treating is not a neutral option”
In 2009, UCSF’s Division of Pediatric Endocrinology got a phone call from the father of a 12-year-old who was assigned female at birth but identified as male.
“He asked if we provided puberty blockers,” says Stephen Rosenthal, M.D., then clinic director for the division. “We had never provided services for transgender people. I was aware they were on the planet, but I thought they just emerged in adulthood and went through transition with hormones and surgery.”

Credit: Elisabeth Fall/UCSF
Rosenthal, a postdoctoral alumnus, started digging but encountered a paucity of academic literature on transgender youth. Finally, he came across a European journal article outlining the “Dutch protocol” – now the foundation of the Endocrine Society’s clinical guidelines for the treatment of transgender youth.
“I began to learn the history and risks faced by transgender individuals and the life-saving benefits of puberty blockers,” Rosenthal says. “Not treating is not a neutral option.”
Such blockers – gonadotropin-releasing hormone (GnRH) agonists – are not new. In the 1980s, GnRH agonists became the gold standard treatment for precocious puberty, to selectively turn off production of sex hormones in very young children exhibiting mature sexual traits. “It’s completely reversible,” Rosenthal says. “You take them off it, and they resume puberty.”
For people with gender dysphoria, the secondary sex characteristics that emerge in puberty – breast development, menstruation, and redistribution of body fat in females; growth of facial and body hair, deepening voice, and enlargement of the genitalia in males – can feel like deformities.
“You can take those kids who are really suffering, put puberty on pause, and give them time to figure out what their gender identity really is,” Rosenthal says. “The beauty of the blockers is that a girl doesn’t have to worry about having an Adam’s apple or a deepened voice. The quality of life for someone blending in according to their gender identity is much better.”
A multidisciplinary approach
The health challenges faced by transgender youth – and the dearth of treatment options – inspired Rosenthal to pursue a unique model of one-stop care.
Launched in 2010, with Rosenthal as medical director, UCSF’s Child and Adolescent Gender Center is the only program in the country with an interdisciplinary team of directors who offer medical, mental health, educational/advocacy, and legal expertise to support gender nonconforming youth and their families.
Clinic patients – who range from as young as three years old through their mid-20s – receive mental and physical evaluation and care. Legal and advocacy staff members are available to advise them on issues ranging from insurance reimbursement and coming out at school, to changing names and genders on documents.
"We’re working with families to support young people in more fully becoming themselves."
— Molly Koren, MSW, Clinical social worker
Rosenthal and his team watch patients for cues – “persistent, insistent, consistent” declarations of who they are, often from a young age, he says – and signs of clinical distress associated with gender dysphoria.
If it appears warranted, patients are prescribed puberty blockers and, for older teens, cross-sex hormones – testosterone or estrogen – to kick-start the puberty that matches their gender identity. Some individuals choose, once they reach age 18, to have genital revision surgery, in which case appropriate referrals are made.
“We’re working with families to support young people in more fully becoming themselves,” says Molly Koren, MSW, a clinical social worker at UCSF Benioff Children’s Hospital San Francisco.
The family-focused approach is key: Parents often need guidance as much as their children.
“When a child says, ‘I’m not the gender you think I am,’ that can be a showstopper,” says Diane Ehrensaft, Ph.D., the Gender Center’s director of mental heath as well as a private-practice psychologist in Oakland. “Some parents say, ‘Not on my watch. No way am I signing off on a medical intervention. When they’re 18 they can do what they want.’ I say, ‘You’re absolutely right, you’re the ones minding the shop, but let me share with you the risk factors of holding back.’”

Credit: Photo by Elisabeth Fall
Easing transitions for kids and parents
Asking his parents if he could turn into a boy for his fifth birthday wasn’t the first – or last – time Shay pushed back at the gender he was assigned at birth. He refused to wear dresses, cut his hair short, and roughhoused with his friends – all boys.
“You think, ‘Oh, he’s just probably a tomboy,’” says his father, Wayne.
Now in eighth grade, Shay, 14, plays flag football and is a soccer goalie on South Bay club teams. He wears athletic shorts, sweats, and shirts, loves video games, banters with his dad, and teases his 11-year-old sister. The only evidence of “difference” from other boys his age is a small circular scar on his arm where a puberty blocker is implanted under the skin.
Five years ago, Shay identified as “gender fluid” on the UCSF Child and Adolescent Gender Center’s spectrum of female (1) to male (10).
Puberty blockers, says Wayne, “bought us time.” Now a firm “10” on the spectrum, Shay transitioned from “she” to “he” in fourth grade and legally shortened his birth name from “Shayna” a year ago. He plans to start taking “T” – testosterone – this year to initiate male puberty.
Wayne credits the Gender Center and Medical Director Stephen Rosenthal, M.D., for easing Shay’s – and his family’s – transition: “He gets it. He takes the time to get to know you and makes sure you have the knowledge and the resources.”
“This is our kid”
Those risks weighed heavily on “Emily” (not her real name) and her husband. Photos in their sun-filled Silicon Valley home show their 10-year-old son and his older sister, “Kelly,” who has the same pre-Raphaelite honey blond hair and bright hazel eyes as her mom.
Five years ago, they were a family with two sons.
“When she was four years old, she asked me why did I make her a boy? And could she go back inside my tummy and come out as a girl? And if she died could she come back as a girl? That just broke my heart,” says Emily (who requested pseudonyms to protect the family’s privacy).
"I was thinking, I can't lose my kid. I don’t care what her gender is. I’ve got to get on the other side of those statistics."
— "Emily," mother of transgender child
A therapist advised them not to confuse Kelly by allowing her to wear dresses, but to compromise with boy’s clothes in flowing, ethnic fabrics and colorful Hawaiian prints. It didn’t help. She was increasingly shy and anxious and wanted everything girly.
One day Emily got a call from her husband, who was in his car listening on the radio to Joel Baum, M.S., the Gender Center’s director of advocacy as well as the director of education and training for the Oakland-based nonprofit Gender Spectrum. “You’ve got to turn on the radio,” he told her. “I think this is our kid.’”
Emily was horrified to learn about the high rates of harassment, school failure, and suicide among transgender youth. “I couldn’t talk about it without weeping. I kept going to all these images in our culture for transgender people, that they’re on the edge, disenfranchised,” she says. “I was thinking, ‘I can't lose my kid. I don't care what her gender is. I’ve got to get on the other side of those statistics.’”
Her path forward, she says, was “unconditional acceptance of my child’s truth.”
The family started regular visits to Gender Center clinics and let Kelly be their guide. She grew her hair long. In third grade, she switched her masculine birth name to a gender-neutral nickname. At age nine, she transitioned socially, becoming “she” to relatives, friends, and classmates.
Intensely private, Kelly wanted no emails to parents, no classroom announcement. Just a quiet switch in pronouns. Her elementary school administrators and teachers – faced with their first transitioning student – were “incredibly supportive,” says Emily, who sought out staff training and put Kelly in a classroom with only one student who knew her from “before”: her best friend.
Now 13, Kelly has a matchstick-sized implant under the skin near her left bicep to suppress the male hormones her body produces. She’s blossomed into a “beautiful, smart, artistic, empathetic, fun kid,” Emily says. “I'm like, ‘Whoo! I hit the jackpot.’ But it was a definitely a process and a journey for our family, and our daughter, to come to understand who she was.”
Building the evidence base
The Gender Center’s patient load – now more than 300, with about 10 new referrals a month – reflects the explosion in the number of transgender youth seeking specialized services across the country, says Rosenthal.
Families come from as far as Alaska, Florida, and Egypt for weekly clinics offered in San Francisco and a new location in San Mateo. A clinic at UCSF Benioff Children’s Hospital Oakland is in the works.
The Gender Center’s approach may be in demand – and the standard of care for persistent gender dysphoria – but it’s not without controversy.
In the May 2015 issue of Pediatrics, one group of critics lambasted the gender-affirming model for reinforcing “the delusions of gender identity-confused children.” Citing the lack of long-term data on medical transitions, the critics called the approach an “ideology-driven social experiment.”
UCSF, along with three other academic institutions with dedicated transgender youth centers, are addressing that lack of evidence with a $5.7-million grant from the National Institutes of Health (NIH).
The five-year study – the first of U.S. transgender youth funded by the NIH – will evaluate the physiological and psychosocial impact of puberty blockers and cross-sex hormones.
“We’re really excited to pool our resources,” says Rosenthal. “This study will help to effectively and safely guide the clinical care of these youth.”
Righting the “wrong” puberty
By age 15, Oliver Bishop was on a dual regimen of testosterone, plus puberty blockers to keep his endogenous estrogen from competing with the male hormones.

Credit: Gabriela Hasbun/UCSF
He came out to his classmates by creating a second Facebook account with his new name, chosen after he asked his mom what it would have been if he had been born male: Oliver, after his great-grandfather.
While he had to endure a second puberty, and he’ll need to take testosterone for the rest of his life, he’s had no second thoughts about transitioning.
The summer after his sophomore year, he had “top” surgery – a double mastectomy and male chest contouring – in San Francisco. To pay for the procedure, which was not covered by insurance, he used earnings from years of showing and selling pigs at the Tuolumne County fair.
“It’s a lot of money for a 15-year-old,” he says of the $8,000 price tag. “But I appreciate it every day.”
His family’s insurance also wouldn’t cover a puberty blocker implant, so Bishop at first chose cheaper but “gnarly” monthly shots. Later, concerned about unknown long-term effects of the blockers, and hating the painful shots, he opted for a hysterectomy at age 16 – performed by the same family doctor who had delivered him.
While Bishop can almost seem blithe at times about his transition, it hasn’t all been smooth. There are still derogatory remarks. His extended family has had a mixed response.
But he doesn’t waste time worrying about the stings. The first in his small town to come out as a transgender person and to medically transition, he’s been a role model for peers who share nontraditional gender expressions. He’s on a glide path to graduation, his grades are high, and he plans to pursue a degree in music education. In June, he’ll undergo the first in a series of “bottom” surgeries to create male genitalia.
His only regret, he says, is not finding UCSF’s Gender Center sooner. “To not go through the wrong puberty, those kids are lucky,” he says. “That’s a team effort. You have to show [gender dysphoria], and parents have to catch it.”
He doesn’t take his parents’ evolution, or their support, for granted. “I couldn’t have done this without them. And I would not have been able to make it without the Gender Center helping me and my parents understand, and medically transition,” Bishop says. “In the rawest form, the center saved my life.”