Levi Gadye, UC San Francisco
Every day, nearly 5 million children in the U.S. wake up not knowing whether they’ll make it through the school day, soccer practice or a sleepover with friends without suffering from debilitating coughing, wheezing and shortness of breath. These children have asthma, and there is no cure. But what if there was a way to predict the chances of a child developing asthma and intervene to prevent it?
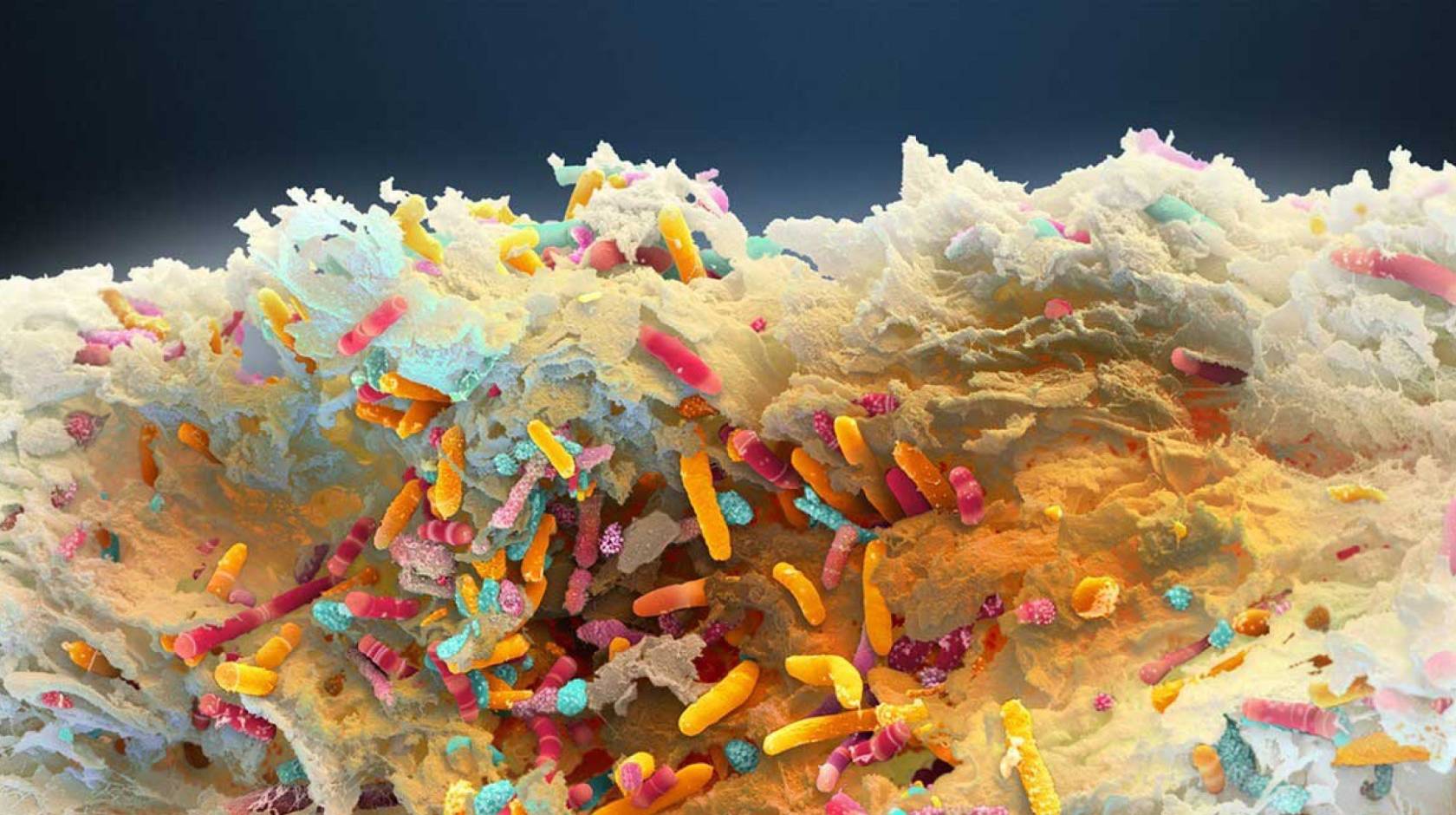
In 2019, UC San Francisco scientists found a link between the gut microbiome — the community of microbes living in the gut — and childhood risk of asthma. They are now charting a new course for treating the disease by focusing on those microbes.
There are microbiomes all over and inside our bodies, from the gut to the mouth, to our skin and airways. The microbes in each microbiome play a big role in our health and, unfortunately, in disease. But an improved understanding of our relationship to these microbes has opened the possibility of treating a variety of human diseases by targeting microbiomes themselves.
“Our goal is to engineer the infant gut microbiome to divert the growing child’s trajectory away from asthma development. We also plan to apply this technology to target airway pathogens and reduce exacerbations for children who already have asthma,” said Sue Lynch, Ph.D., director of the UCSF Benioff Center for Microbiome Medicine (BCMM) and leader on the project. “We’re aiming to have a therapy ready for human clinical trials in under 5 years.”

Susan Lynch, Ph.D.
How to train the immune system
Lynch has partnered with Nobel Laureate Jennifer Doudna, Ph.D., as well as Jill Banfield, Ph.D. — both CRISPR gene editing pioneers at UC Berkeley and the Innovative Genomics Institute (IGI) — to precisely modify asthma-causing genes in the microbiome without disturbing the microbiome’s beneficial functions.
The infant microbiome is uniquely positioned for effective interventions that last, Lynch explained. The asthma therapy she’s working on modifies the infant gut microbiome, which in turn trains the developing immune system to function healthily over the course of a lifetime.
By piloting this approach in a known example of a microbiome-related condition, the group intends the pave the way for treating many other conditions, ranging from ulcerative colitis to periodontal disease and multiple sclerosis.
“The combination of UCSF's incredible clinical infrastructure and the science facilities within the Benioff Center for Microbiome Medicine make us uniquely poised to push the boundaries of translational human microbiome research,” said Lynch.


