Linda Wang, UCLA

In June 2018, actor Hirotaka Matsunaga was supposed to be two weeks away from opening night of “The Swords of Sorrow: BURAI II,” a play set in 1800s Japan. The 39-year-old had been cast as the lead. It was the big break he had been working toward since he moved to the U.S. from Japan more than 20 years ago to pursue his dreams.
But his cancer diagnosis and an unsuccessful course of chemotherapy had shut down the play.
“Around November 2017, I had acute pain in my stomach for weeks, and it got so bad that it became difficult to eat,” Matsunaga said.
After a particularly agonizing dinner, he checked himself into a hospital where doctors found a large mass near his stomach. The mass turned out to be follicular lymphoma, a type of non-Hodgkin’s lymphoma.
Over the next four years, Matsunaga endured two courses of chemotherapy in combination with immunotherapy, but the cancer always returned and eventually transformed into a more aggressive, B-cell non-Hodgkin’s lymphoma.
That’s when Matsunaga’s physician, Dr. John Timmerman, a professor of hematology/oncology in the David Geffen School of Medicine at UCLA, recommended he enroll in a chimeric antigen receptor, or CAR, T cell therapy trial led by members of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA and UCLA Health Jonsson Comprehensive Cancer Center for patients with relapsed or refractory B-cell non-Hodgkin’s lymphoma.
An avid martial arts practitioner, Matsunaga has always believed the best way to overcome any obstacle is to wholeheartedly commit to taking decisive action. Still, the thought of participating in a clinical trial gave him pause.
“I had to sleep on it for a few nights and talked with my wife and mother about the risks,” he said. “But ultimately, I knew this was the way to go because patients who were in the trial before me were having good results.”
In August 2022, he started treatment in the phase 1, first-in-human clinical trial of a cutting-edge CAR-T cell therapy co-led by Dr. Yvonne Chen and Dr. Sarah Larson.
Stronger and smarter CAR-T cells
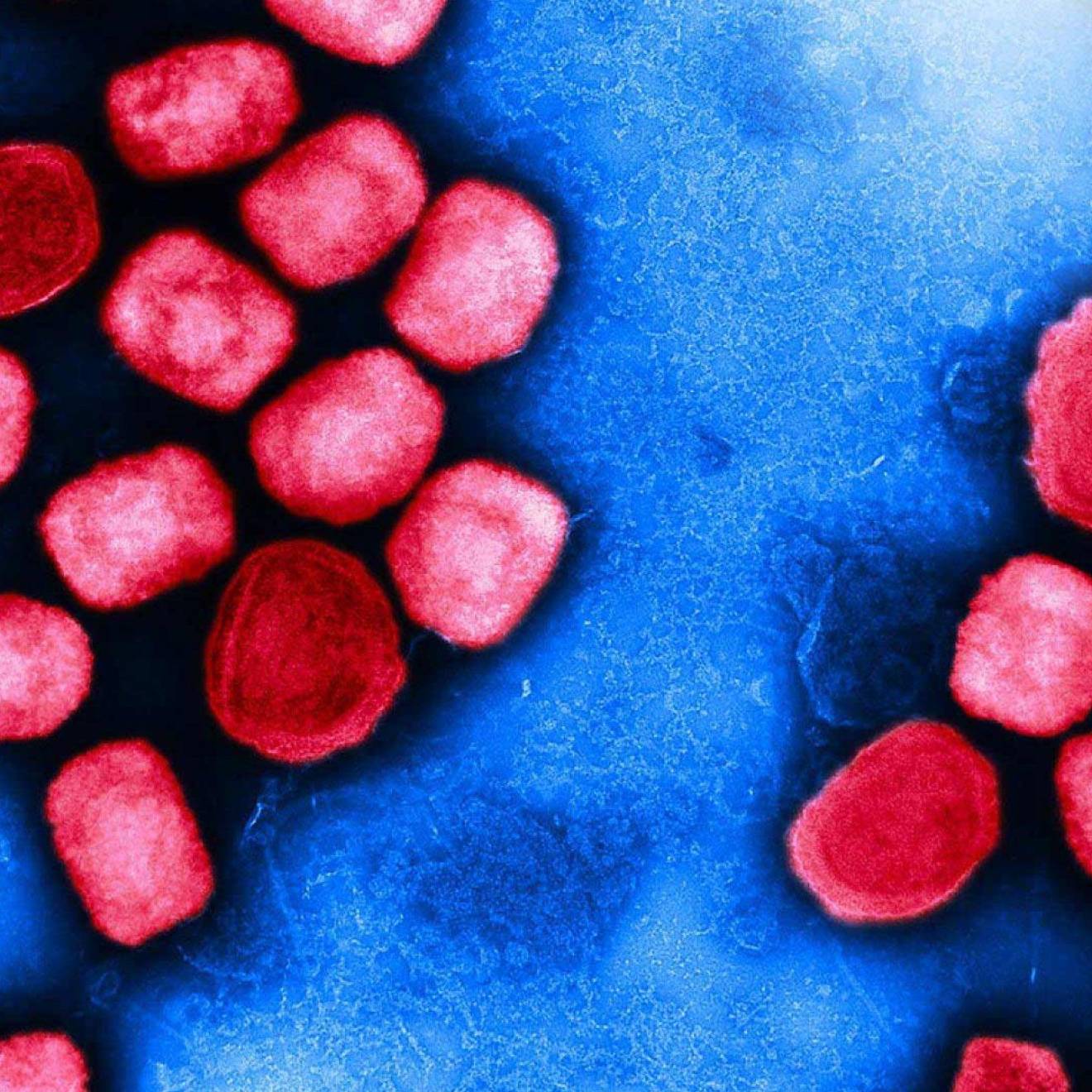
This experimental treatment involved collecting Matsunaga’s immune cells, called T cells, modifying them with CARs — special cancer-recognizing receptors — and then giving them back to him by infusion. This process allows the modified T cells to find and kill cancer cells.
This approach uses CARs that are considered both “smarter” and “stronger” than those used in other therapies because they’ve been designed to recognize two targets, called antigens, on lymphoma cells — CD19 and CD20 — instead of just one.
CAR-T cell therapies have revolutionized cancer care, but resistance and relapse can occur, partly because tumors have various ways to defend themselves such as by losing the specific antigen that’s targeted by the CAR-T cells, a process known as antigen escape.
“In our approach, we’re equipping T cells to launch a bilateral attack, so the tumor would have to lose both of the antigens to successfully escape, making it much more difficult for the tumor to evade therapy,” said Chen, a professor of microbiology, immunology and molecular genetics in the UCLA College who designed the bispecific CAR that’s being evaluated in the trial.
Today, after 20 months in the study, Matsunaga has been in remission for 18 months.
“I don’t have any symptoms at all, so I’ve been exercising more and getting back into martial arts,” he said. “I feel like myself again.”
Of the 11 patients treated so far in this ongoing trial, 10 responded to the treatment and eight achieved a complete response, meaning their tumors went away.
Equally noteworthy, none of the patients experienced neurotoxicity, a side effect of conventional CAR-T cell therapies that approximately 40% of patients experience and that in rare cases can be fatal.
Larson, an associate professor of hematology/oncology at the Geffen School of Medicine, said: “Getting these results is so important because we really need to make sure that products like this one can be offered to all patients — especially those who’ve run out of other treatment options. Expanding access to CAR-T cell therapy in general is really the next phase.”
The technology has been licensed to a company named ImmPact Bio, which has been granted a Fast Track Designation by the FDA — meaning the therapy has a chance to receive accelerated approval. The company has started its own multi-site clinical trial with UCLA being the first site.
Chen and Larson are now developing a dual target CAR-T cell therapy for patients with multiple myeloma and pursuing strategies to help make these treatments more widely available and cost-effective for patients.
The next chapter
Now 45, Matsunaga is taking new acting roles without the worry of relapsing and the toll of weekly chemotherapy infusions.
“I feel like I’ve lost years of my life to this disease,“ he said. “But I hope my story offers comfort to others by letting them know you can live a fulfilling, exciting life after cancer.”
This clinical trial is funded in collaboration with the UCLA Health Jonsson Comprehensive Cancer Center, the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA, the National Institutes of Health and the Parker Institute for Cancer Immunotherapy.