Stephen P. Wampler, Lawrence Livermore Lab
Buoyed by several dramatic advances, Lawrence Livermore National Laboratory scientists think they can tackle biological science in a way that couldn't be done before.
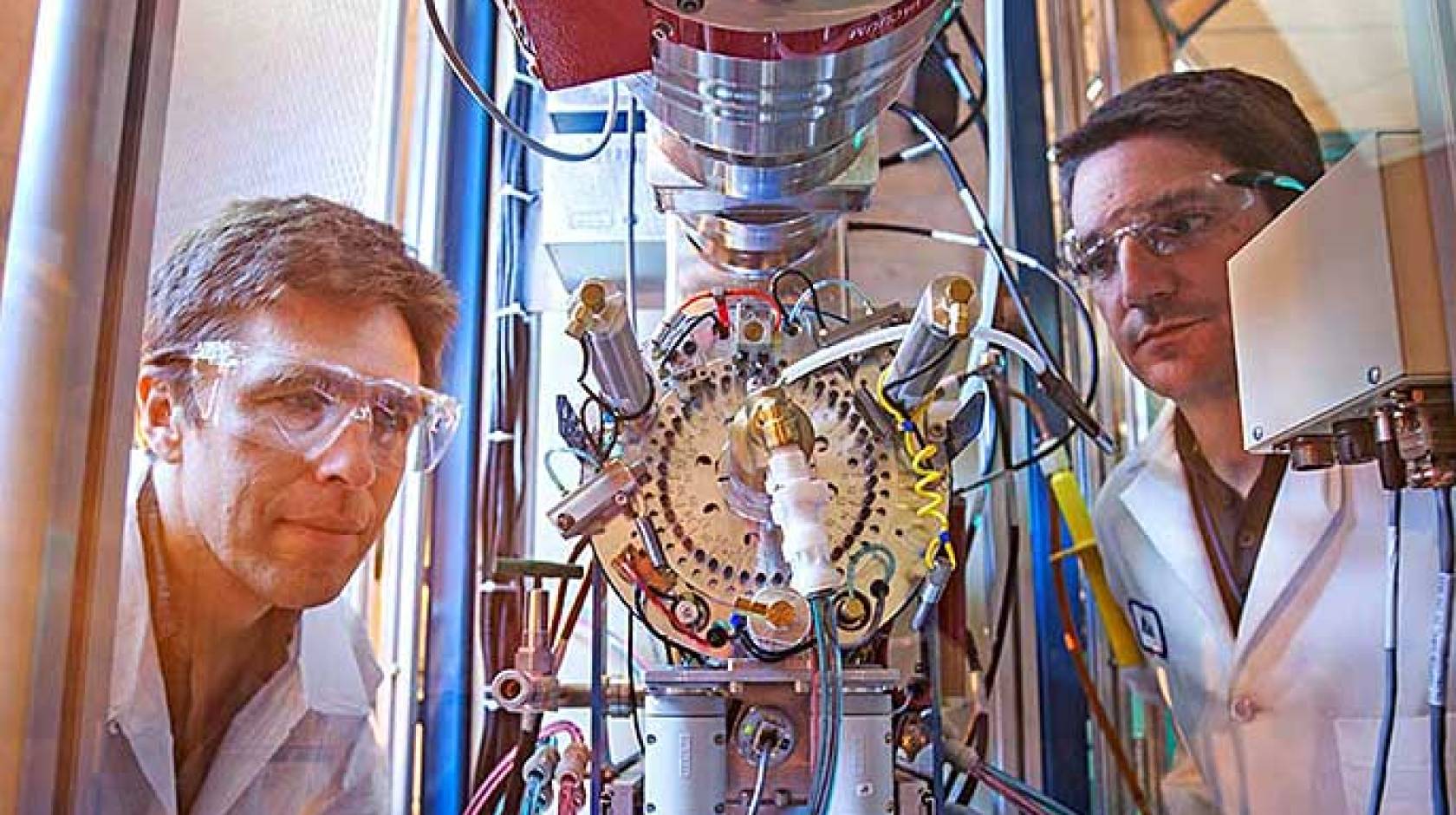
Over the past two years, lab researchers have expedited accelerator mass spectrometer sample preparation and analysis time from days to minutes and moved a complex scientific process requiring accelerator physicists into routine laboratory usage.
Ken Turteltaub, the leader of the lab's Biosciences and Biotechnology Division, sees the bio AMS advances as allowing researchers to undertake quantitative assessments of complex biological pathways.
"We are hopeful that we'll be able to quantify the individual steps in a metabolic pathway and be able to measure indicators of disease processes and factors important to why people differ in responses to therapeutics, to diet and other factors," Turteltaub said.
Graham Bench, the director of the lab's Center for Accelerator Mass Spectrometry, anticipates the upgrades will enable lab researchers "to produce high-density data sets and tackle novel biomedical problems that in the past couldn't be addressed."
Ted Ognibene, a chemist who has worked on AMS for 15 years and who co-developed the technique that accommodates liquid samples, also envisions new scientific work coming forth.
"We previously had the capability to detect metabolites, but now with the ability to see our results almost immediately for a fraction of the cost, it's going to enable a lot more fundamental and new science to be done," Ognibene said.
Biological AMS is a technique in which carbon-14 is used as a tag to study with extreme precision and sensitivity complex biological processes, such as cancer, molecular damage, drug and toxin behavior, nutrition and other areas.
Among the biomedical studies that will be funded through the five-year, $7.8 million National Institutes of Health grant for biological AMS work is one to try to develop a test to predict how people will respond to chemotherapeutic drugs.
Another research project seeks to create an assay that is so sensitive that it can detect one cancer cell among one million healthy cells. If this work is successful, it could be possible to evaluate the metastasis potential of different primary human cancer cells.
Lab biomedical scientist Mike Malfatti and two researchers — Paul Henderson, an associate professor, and Chong-Xian Pan, a medical oncologist — from the University of California, Davis Comprehensive Cancer Center, are using the AMS in a human trial with 50 patients to see how cancer patients respond or don't respond to the chemotherapeutic drug carboplatin. This drug kills cancer cells by binding to DNA, and is toxic to rapidly dividing cells.
The three researchers have the patients take a microdose of carboplatin — about 1/100th of a therapeutic dose — that has no toxicity or therapeutic value to evaluate how effectively the drug will bind to a person's DNA during full dose treatment.
Within a few days of patients receiving the microdose, the degree of drug binding is checked by blood sample, in which the DNA is isolated from white blood cells, or by tumor biopsy, in which the DNA is isolated from the tumor cells.
The carboplatin dose is prepared with a carbon-14 tag. The DNA sample is analyzed using AMS and the instrument quantifies the carbon-14 level, with a high level of carbon-14 indicating a high level of drug binding to the DNA.
"A high degree of binding indicates that you have a high probability of a favorable response to the drug," Malfatti said. "Conversely, a low degree of binding means it is likely the person's body won't respond to the treatment.
"If we can identify which people will respond to which chemotherapeutic drug, we can tailor the treatment to the individual.
"There are many negative side effects associated with chemotherapy, such as nausea, loss of appetite, loss of hair and even death. We don't want someone to receive chemotherapy that's not going to help them, yet leave them with these negative side effects," he added.
Malfatti, Henderson and Pan also are using the AMS in pre-clinical studies to investigate the resistance or receptivity of other commonly used chemotherapeutic agents such as cisplatin, oxaliplatin and gemcitabine.
Another team of researchers, led by Gaby Loots, a lab biomedical scientist and an associate professor at the University of California, Merced, wants to use AMS to measure cancer cells labeled with carbon-14 to study the cancer cells' migration to healthy tissues to determine how likely they are to form metastatic tumors.
While today's standard methods can detect tumors that are comprised of thousands of cells, the team would like to develop an assay with a thousand-fold better resolution — to detect one cancer cell among 1 million healthy ones.
"The sensitivity of AMS allows us to develop more accurate, quantitative assays with single-cell resolution. Is the cancer completely gone, or do we see one cell worth of cancer DNA?" Loots noted.
Some of the questions the team would like to answer are:
- why certain cells metastasize?
- how do cells metastasize?
- what new methods can be developed to prevent metastasis?
"Tumors shed cells all the time that enter our circulation. We would like to find ways to prevent the circulating tumor cells from forming metastatic tumors," Loots continued.
As a part of their research, the team members hope to determine whether cancer cells with stem-cell-like properties form more aggressive tumors.
"We're going to separate the cancer cells into stem-cell-like and non-stem-cell-like populations and seek to determine if they behave differently," said Loots, who is working with fellow lab biomedical scientists Nick Hum and Nicole Collette.

