Note: This article has not been updated since April and some best practices and guidelines have changed. To view up-to-date information on the coronavirus in California, please visit https://www.cdph.ca.gov/covid19 or visit https://www.universityofcalifornia.edu/coronavirus for information about UC’s response.
The nonstop flow of information about the novel coronavirus and COVID-19 can spin you into confusion. Conflicting research and rumors abound.
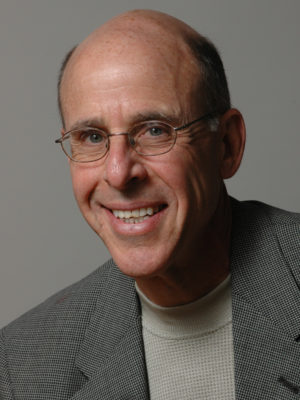
What will really keep you safe? What should we actually worry about (and what’s just overkill)? We asked our community for their most pressing questions and put them to Dr. John Swartzberg, professor emeritus of public health at UC Berkeley to get some clarity.
Of course, there are still many aspects of the virus that haven’t been studied yet. Research and recommendations are evolving quickly. But four tips from Dr. Swartzberg will stay the same — and remain vital for dealing with the virus:
- Wash your hands;
- Don’t touch your face (unless you have just washed your hands);
- Stay at least six feet away from anyone who is not in your immediate household; and
- It’s OK to be excessive if it makes you feel safe and more comfortable.
To get deeper into the latest science and guidance on how to protect yourself around the coronavirus, read on. Dr. Swartzberg’s answers are condensed below.

How long can the virus survive on clothing?
A New England Journal of Medicine study (co-authored by UCLA researchers) is the main resource for how long the virus can live on inanimate objects thus far. It found the virus could live for 4 hours on copper, 24 hours on cardboard and 72 hours on plastics and certain metals. We still need to study clothing, but Swartzberg suspects it would be similar to cardboard, as it’s also porous.

How concerned should you be about disinfecting groceries or packages delivered to the house?
We should be prudent about packaging. If you receive a package in the mail and don’t have to open it right away, just put it aside — and then go wash your hands. After 72 hours, you can open and unpack it with no worries. Same for non-perishable groceries. If it is a perishable item, let it sit in your fridge for three days without touching it. If it’s a grocery item you need to open or use right away, you may want to wash the packaging with soap and water or clean it with a disinfectant.
Should we be washing fruits and vegetables with something other than plain water?
“How long the virus can live on organic material hasn’t been studied yet. If it's something you can cook, don't worry about it, because the cooking will kill the virus.”
What about salad greens or other produce you will be eating raw? This is not a food-borne disease and there’s no evidence that eating the virus will infect you. There is a theoretical possibility that when the food is in your mouth, you could aspirate it into your lungs but “it’s quite a stretch.”
If you are nervous, you can create a food-grade bleach solution by diluting it with water but be very careful to get the proportions right and rinse your fruits/veggies with plain water afterwards. Otherwise you risk causing more harm than good by ingesting bleach.

If I’m cleaning countertops, light switches, faucets, etc., with a good old fashioned soap and water mix. Must I scrub each for 20 seconds like I do with my hands? Or can I simply spray and wipe?
“One of the nice things about this virus, if there’s anything nice about it at all, is that soap actually kills it — it doesn’t just escort the virus off you and down the drain. Soap and water truly is one of the best ways for getting rid of the virus in your home. But the soap does need time to work,” Spray or soap up surfaces and/or items in your home, scrub a bit and then let it sit for a few minutes before washing or wiping off. If there’s organic matter on a countertop, scrub that off first.
How many surface touches can the virus survive? For instance: Someone coughs on their hand, delivers your mail, then you put that mail on the countertop, and later touch that countertop and put your hand to your face, could you possibly contract the virus?
“The answer is that we don’t know — it hasn’t been studied.” But with each touch, you transfer less and less virus. We don’t know at what point the amount of virus on that inanimate object is so low that you can’t get infected, however. “I think the reasonable thing to do is if something you’ve done raises in your consciousness the possibility that you could have transferred the virus to your hands, go wash your hands. I’d rather see people err on the side of using soap and water on their hands very frequently.”

Can our pets get COVID-19? If someone who is infected pets my dog could I get infected through transmission on their skin or coat?
It’s now documented that a small number of cats and dogs, whose owners had COVID-19, contracted the disease. Although it lives in their nose and mouth, “what we don’t know is whether they can then transmit it to other humans.” It’s very unlikely, as the virus does not multiply well in our pets.
As for whether we should abstain from touching pets that aren’t our own?
“If I have COVID-19 and sneeze on my dog, and someone immediately pets my dog and brought their hand to their mouth or nose, it’s possible they could get infected.” This has not been studied.
Let’s talk about high-risk groups. Why are those with diabetes or with heart problems more at risk? Does that mean your risk is higher if you have high blood pressure?
In general, people living with diabetes don’t handle infection as well as those without diabetes. The heart and lungs are very closely connected, and since COVID-19 is a lung infection, the stress it puts on the heart is very significant. Conversely, when the heart starts to fail, the lungs fill with fluid. The data from China suggests high blood pressure is clearly a risk factor.

What should we know about wearing masks in public places?
The CDC now recommends wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain, mainly so that those who are asymptomatic or pre-symptomatic do not transmit the virus. Although the effectiveness of homemade masks hasn’t yet been studied, there is good evidence that wearing a mask markedly reduces the quantity of droplets you put forth.
As for N95 or surgical masks, health care professionals need them the most. To be the most effective, they need to be fit tested by professionals. Without this, you’ll be sucking in air through the edges of the mask. They are also very uncomfortable, and get hot quickly.
Masks can give people a false sense of security, leading them to believe they no longer need to stay six feet away from others while wearing them. “We're frightened to death about this virus and we're looking for anything we can do to prevent getting infected and one of the tools we have is to wear a mask. It may help somewhat but I don't think science tells us that it's going to help nearly as much as staying at least six feet apart from people.”
Can the virus “hang out” in the air? I’m confused by all the conflicting answers on this.
For better or worse, biology is not “yes” or “no,” so it’s hard to give a definitive answer. That’s why whether or not this virus is “airborne” is a contentious topic.
However, Swartzberg doesn’t believe that the virus will end up widely considered “airborne,” like measles and chickenpox. Here’s why: Pathogens are all assigned reproductive numbers (R0). Measles has a high R0 of 12-18. This means that for every one person that has measles, they are likely to infect 12-18 people. This coronavirus, SARS-CoV-2, has an R0 somewhere between 1.5 and 3.5, most likely. This tells him that it’s not nearly as contagious as those airborne diseases. It’s probable that there are instances when it is transmitted through the air, but it’s certainly not as transmissible as when it spreads through droplets (i.e., someone coughing or sneezing within six feet of you or if you touch a surface contaminated with the virus).

Where do you draw the line on social distancing? If someone is an “essential worker” and needs to be interacting with the public every day, should they be socially distancing from their families? Should grandma not see her grandkids?
“These are tough decisions for families and public health professionals, and doctors can't give absolute advice, or a right or wrong answer.” He gives a personal example.
He and his wife, both over 70, have not hugged their children or grandchildren for weeks (except virtually) despite living only 10 minutes away. “It’s horrible,” he adds, but they know they are high-risk due to their age.
In the end, these decisions are personal. Swartzberg has friends on the front lines who have sent their partners and families to live elsewhere. He knows still other physicians who come home every day, go to the laundry room, take off their work clothes and put them in the washing machine, shower, wash their hair and only then hug their children. Could they be asymptomatic carriers? Perhaps — but they have decided to take that tiny bit of risk, especially since children seem not to get seriously ill with the virus. It’s an individual decision of what is tolerable for your family.
If you had to give your best guess, are we likely to be back at work, school and socializing by June 1? Are we going to be able to go on a summer vacation?
We will likely take a phased approach to going back into the world. Those of us at the least risk of getting seriously ill and/or dying may go back to work first. Those who are elderly or living with chronic diseases should still shelter in place. He believes this could start in California sometime in May.
We don’t know if it will be safe to travel this summer. He thinks flying represents a real hazard and doesn’t recommend doing so this summer — along with going to crowded concerts or sports games: “I’d take a road trip instead.” And no cruises.

How will we know if these containment measures are working? What statistics are we looking for to indicate that COVID-19 is no longer a dramatic public health concern?

We have excellent computer models — and we are pretty much on the curve as predicted. If in the following days or weeks, our numbers haven’t increased in the same way that it shows on the model, it will suggest that sheltering in place works. If we never get to the peak shown in the model, or we start to decline earlier than the model suggests, we also know sheltering in place works. The numbers are going to go up in California, but he doesn’t think they’ll go up as projected. He also warns that if things get better but we stop intervening too soon, it will only get worse again.
Will there be a test to see if we’ve already had COVID-19 and would it be widely used?
There is an antibody test that will tell us if we were infected — even if we never got the disease of COVID-19 and remained asymptomatic. Not everyone will get this test — instead a random sampling will allow us to approximate how many people contracted the virus in total.

Will the vaccine have to be given every year, like the flu vaccine?
Probably not. The genetics of the virus hasn’t changed in the past few months, so its mutations must be dying off and not succeeding. Everything up until now suggests the virus won’t change very much, and Swartzberg is optimistic that it will stay that way.
What are the top questions you have that have not yet been answered in the scientific community?
- What is the relative likelihood for different means of transmission? We need that information to pinpoint what we should be doing, and what we don’t have to worry about. “If we didn't need to worry about a lot of things, our lives would be a lot better — because right now, we worry about everything.”
- How many people have been infected, and where are they? We’re currently applying measures diffusely across the country and world. If we had the data to predict that some areas would get hit harder than others, we could focus attention and distribute resources accordingly. If we knew who was getting extremely sick, we could also create better public health interventions for them.
- What therapeutics will work? “If we had an antiviral drug that worked, it would be a game changer. Certainly if we had a vaccine that worked, the ballgame would be over.”
- Do the antibodies we produce from being infected protect us against reinfection? There are some diseases which we never get again but there are others in which the antibodies are either not protective, or only protective for a short while.