Rebecca Vesely, Special to UC Newsroom

UC Irvine Health clinicians have developed novel strategies to screen, detect and intervene to prevent life-threatening blood clots.
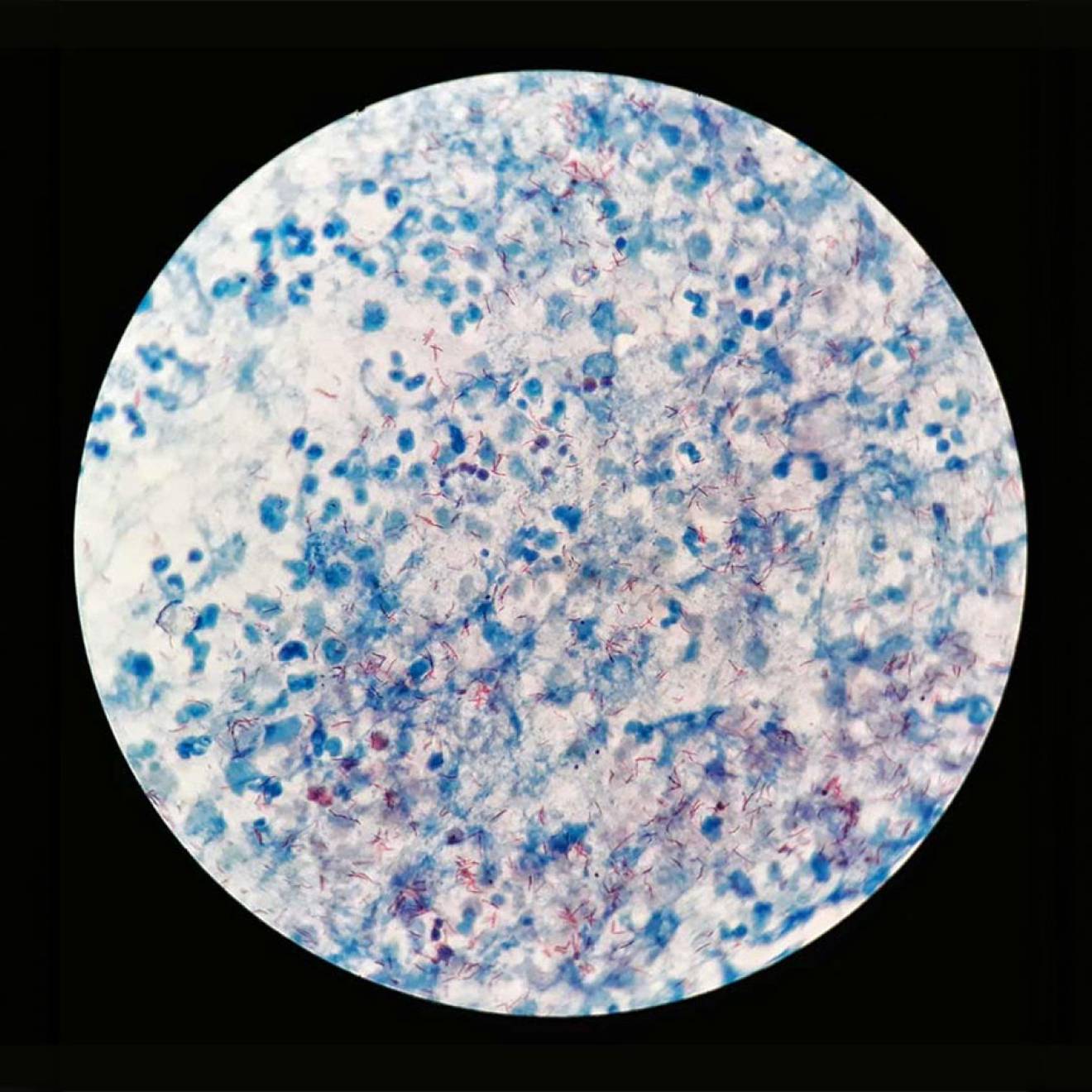
Blood clots are a leading cause of preventable deaths in hospitals nationwide and are often overlooked. Among the most deadly of these conditions is venous thromboembolism, VTE, which occurs when a blood clot that develops in a deep vein of the leg or pelvis (called a deep vein thrombosis) dislodges and travels to the lung to form a pulmonary embolism.
A challenge hospitals face is making sure patients receive appropriate screening and treatment for VTEs to reduce risks. In the U.S., about two-thirds of all VTE events result from hospitalization, but only one-third of patients at risk for developing VTEs in the hospital receives adequate prophylactic treatment. Patients over age 40 and on bed rest from surgery or illness are especially at risk for developing VTE. As a result of appropriate screening and interventions, from July 2012 to July 2013, UC Irvine had no preventable cases of VTE out of a total of 114 VTE cases.
UC Irvine Medical Center is one of 13 California public hospitals that chose VTE as a Delivery System Reform Incentive Program project. DSRIP is a novel, pay-for-performance initiative in which California’s 21 designated public hospitals receive Medicaid dollars in exchange for meeting pre-set milestones.
Accelerating improvements
While reducing VTE was a focus at UC Irvine prior to the start of the DSRIP, its inclusion gave providers the green light to accelerate the program and make it a priority, said UC Irvine Medical Center Chief Nursing Officer Karen Grimley. UC Irvine also is participating in a UC-wide collaborative on VTE funded by the UC Center for Health Quality and Innovation.
“It’s improving our mortality and improving additional services beyond the walls of the hospital,” Grimley said. “It’s a win-win for us and for patients.”
Pulmonary embolism is the most common preventable cause of hospital-related death. Nationally, there are about 1 million cases of VTE annually and, of those, some 300,000 die from the condition.
UC Irvine is one of the few hospitals nationwide that screens all patients for VTE risk. As of 2012, the hospital’s electronic medical record requires a standardized, evidence-based VTE assessment on patients and guides providers to choose appropriate prophylaxis.
Based on this risk assessment, physicians order proper preventative treatment, ranging from getting patients up and walking to wearing graded pressure socks to taking anticoagulant medications. All registered nurses receive training on VTEs and are responsible for implementing prevention strategies.
Another important component of VTE response is improving the safety of anticoagulation care. As of 2013, pharmacists at UC Irvine Medical Center manage all patients who receive the blood-thinning medication warfarin (Coumadin) during their inpatient visits. Pharmacists also verify that patients discharged with warfarin have scheduled follow-up appointments with outpatient providers. This is an important care transition program aimed at improving medication adherence and outcomes while reducing preventable readmissions.
Enormous effort
Being able to screen all patients for VTE and monitor and track them over time takes enormous effort that would not be possible without DSRIP, said Dr. Alpesh Amin, UC Irvine Health professor of medicine and leader of the VTE program.
“You constantly have to keep a level of education going because you always have new people coming into the organization,” Amin said. “We don’t want it to be dependent on the individual but instead should be process-driven.”