Laura López González, UC San Francisco

Ten-month-old Amir Hayden sits on his mother’s lap inside a sound-proof booth at UCSF Benioff Children’s Hospitals audiology clinic in Oakland, as audiologist Sarah Coulthurst, MS, takes him through a hearing test of different tones. He doesn’t react.
Amir’s mother, Alisa Ellingberg, already suspects something is wrong.
Amir has just recovered from bacterial meningitis, a potentially deadly infection that causes swelling around the brain and spine. Up to 35% of children who survive the illness are left with hearing loss, partly because the infection can result in damage to the inner ear’s cochlea, the organ that carries sound to the auditory nerve and up to the brain.
“It kicked us into high gear,” says Coulthurst, co-director of UCSF Benioff Oakland’s cochlear implant team, of Amir’s hearing test.
Her co-director, Dylan Chan, MD, PhD, UC San Francisco professor in residence and ears, nose and throat surgeon, quickly sees Amir and orders more scans as a multidisciplinary expert team assesses the boy. The scans confirm meningitis has left Amir deaf. Damage from the infection now risks entombing his cochlea nerve in a bony shell within days, permanently cutting off his only chance to perceive sound again with a surgically embedded device known as a cochlear implant. It’s a race against time.
“We have to implant him on Monday,” Coulthurst remembers Chan saying.
The team diagnoses and prepares Amir to receive a cochlear implant in each ear in just eight days – a hospital record.
UCSF researchers helped invent the cochlear implant in the 1970s. And by 1981, UCSF professor emeritus in Otolaryngology Michael Merzenich, PhD, had developed the first true precursor to the modern device. In 1990, a similar device was approved for use in children.
Cochlear implants bypass damaged portions of the hearing system and directly stimulate the auditory nerve, which carries that information to the brain that then learns to interpret it.
Laughing and smiling at his mother’s voice
On Sept. 29, 2022, after Amir had healed from surgery, Coulthurst turned on his cochlear implants.
“He hadn’t heard for about a month, and his mom said the hardest part during that was watching him wonder what was going on,” Coulthurst remembers. “The minute he was able to detect sound again, you could see he was almost relieved.”
She continues: “With the second ear, he really responded, laughing and smiling as he listened to his mom’s voice and making that connection as he watched her speak to him.”

If UCSF’s Merzenich helped invent the cochlear implant, UCSF Benioff Oakland audiologist Adeline McClatchie, CCC-A, developed the West’s first comprehensive multidisciplinary model to get it into the hands of families with children who are severely hard of hearing or, like Amir, deaf.
Hailing from the U.K., McClatchie joined the Oakland hospital in 1967 in the wake of a national rubella outbreak that had left an unusually high number of babies with hearing loss. In the East Bay, many parents were navigating diagnoses without support.
“These were often single mommies of a deaf baby – they didn’t have social lives,” she remembers. “My mummies were very lonely girls.”
McClatchie’s care for the children and their mothers went beyond hearing tests, and included parenting help, meal planning (“There were a lot of Irish stews made during that time.”) and working with the children’s teachers to set goals: “I integrated the audiology clinic into the schools.”
She wanted the children to be able to communicate, whether by speech, signing or a mix of both. So, she followed the development of a cochlear implant for children with anticipation. But which children would the device work for? How would their families pay for it? How would they learn to use it? And what resources could be developed to help them? McClatchie wanted to bring a group of experts together to think these and other questions through but needed funding to do it.
First-of-its-kind model of care
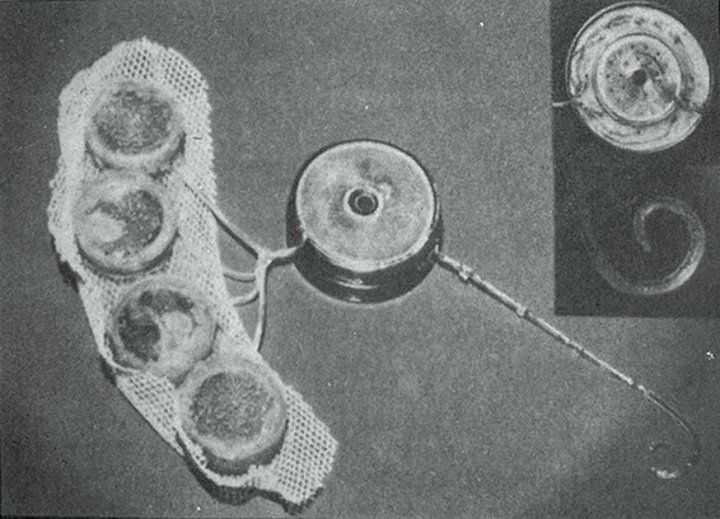
An early prototype of the implantable components of a cochlear device, which was developed at UCSF. Credit: UCSF
It was 1990 and a London-bound airplane was crossing the Atlantic Ocean. On board, McClatchie rose to stretch her legs and met another passenger doing the same. She was telling him about her hopes of providing cochlear implants to kids when the man revealed he was a prominent advocate for the Deaf with a large foundation.
“Send me a proposal,” he suggested.
“Just give me a minute,” McClatchie remembers saying and dashed to her seat to retrieve a funding proposal for Oakland’s future cochlear implant program. “My husband always said to carry a research proposal in my back pocket.”
The foundation awarded McClatchie a grant, funding one of the first teams of UCSF Benioff Oakland surgeons, audiologists, speech pathologists, psychologists, radiologists, and local teachers of the Deaf. Together, they met in the hospital basement, weighing cochlear implant cases and coordinating care – often over a local favorite, Zachary’s Pizza.
Soon, clinicians and teachers of the Deaf from all over Northern California were bringing patient cases to McClatchie for assessment as part of her whole-child model. Together, they reviewed cases, including each potential patient’s support system, family unit and school setup, says Coulthurst, who took over the cochlear implant team in 2008. “They wanted all those different expert perspectives about what, realistically, we could hope to achieve with a cochlear implant, and how our team could support each child to communicate no matter what treatment they received.”
Years later, the faces may have changed, but the team of experts continues to meet, ensuring patients like Amir have wraparound care and support on their cochlear journey.

‘All the resources came to me’
In East Oakland, Amir babbles away as he plays on the gray-speckled carpet of his grandmother’s living room. It’s been almost two years since Amir received his cochlear implants. In the corner, the room opens to a large play area filled with cubby holes, a play kitchen and tiny tables. This is where, most days, Amir joins other children as part of his “gammy’s” daycare. On this day, as his mom looks on, he notices a brightly colored baton in a basket of toys. He picks it up and waddles to Alisa, thrusting the baton towards her.
“Green,” Alisa says, pointing to the baton’s cap. Almost as quickly, she forms her thumb and forefinger into a pincher shape, moving them side-to-side. “Green,” she repeats in American Sign Language.
He echoes her aloud, signing back.
After Amir’s cochlear implants were turned on, the pair was sent home with tools to help his brain learn how to listen with his implants and understand new sounds. UCSF Benioff Oakland speech therapist Molly Walker conducts weekly teletherapy video visits with Alisa, coaching her on how to help Amir learn to use the implants and also connecting her to resources like teachers and schools.
“It’s a parent coaching model because parents and caregivers are the No. 1 language teachers for children,” explains audiology program clinical liaison Joy Kearns, MS, CCC-SLP, LSLS. “We’re not just taking care of the kid, and we’re certainly not just taking care of ears.”
Mother and son will go for six-month checkups at the UCSF Benioff Oakland audiology department until Amir is 21.
Although Amir can comprehend speech through his implants and wears them religiously, he still attends classes for the Deaf, where he learns to sign, before attending after-school care with hearing children. Alisa hopes experiences like this will help her boy navigate two worlds as he grows.
“I want him to recognize that he is still a Deaf person, even though he can ‘hear’ with cochlear implants,” Alisa says. She too takes sign language classes with Amir’s teacher, just another of the whole-family services that are now part of the model McClatchie’s team developed.
“That’s what’s so great about his journey,” Alisa says. “Everything, all the resources, came to me. I didn’t have to go searching for anybody because all these people were coming to me to help him because they wanted him to succeed.”
McClatchie went on to help develop the State of California standards for pediatric cochlear implants and advocated for Medi-Cal to cover the devices. For nearly three decades, UCSF Benioff Oakland was one of the only hospitals in Northern California that met state standards to implant Medi-Cal patients.
Today, thanks in part to recent financial support from the Panda Cares Center of Hope, UCSF clinician-researchers continue to pioneer new research to support deaf and hard-of-hearing children to communicate, for instance uncovering new ways that genetics influence deafness and addressing barriers to care among communities of color.
“I was a lone violinist in the ’70s and we became a quartet of clinicians and therapists in the ’80s and the ’90s … but there was one glaring omission,” McClatchie reflects. “We needed a conductor.”
“Research, data collection, is the binding element of any program,” she continues. “With the merger of UCSF Medical Center and Benioff Children’s Hospital Oakland, we now glue together a whole orchestra of care for the deaf and hard of hearing child.”
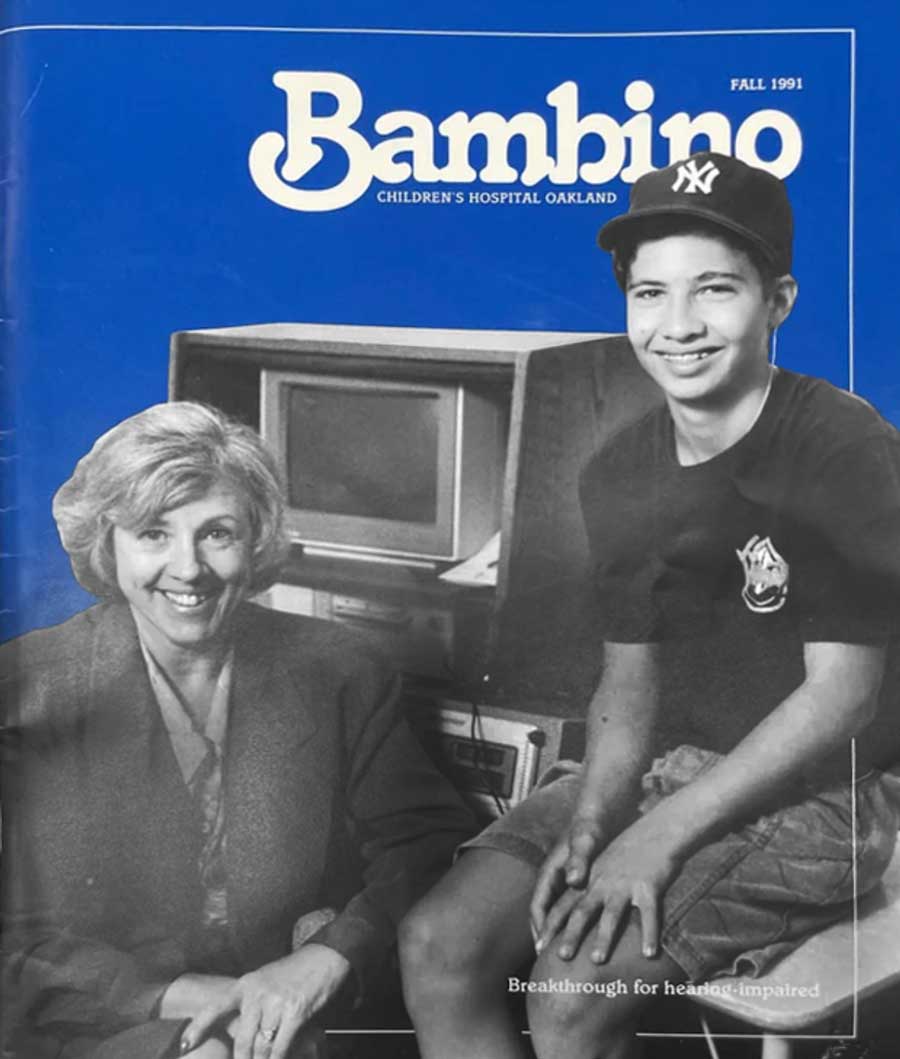
Adeline McClatchie (left) on the cover of the Fall 1991 issue of the Bambino, a quarterly newsletter featuring news about patients, physicians and happenings at UCSF Benioff Children’s Hospital Oakland (then Children’s Hospital).
To her right is Cameron Garberoglio, the first child to receive a cochlear implant at UCSF Benioff Oakland.

