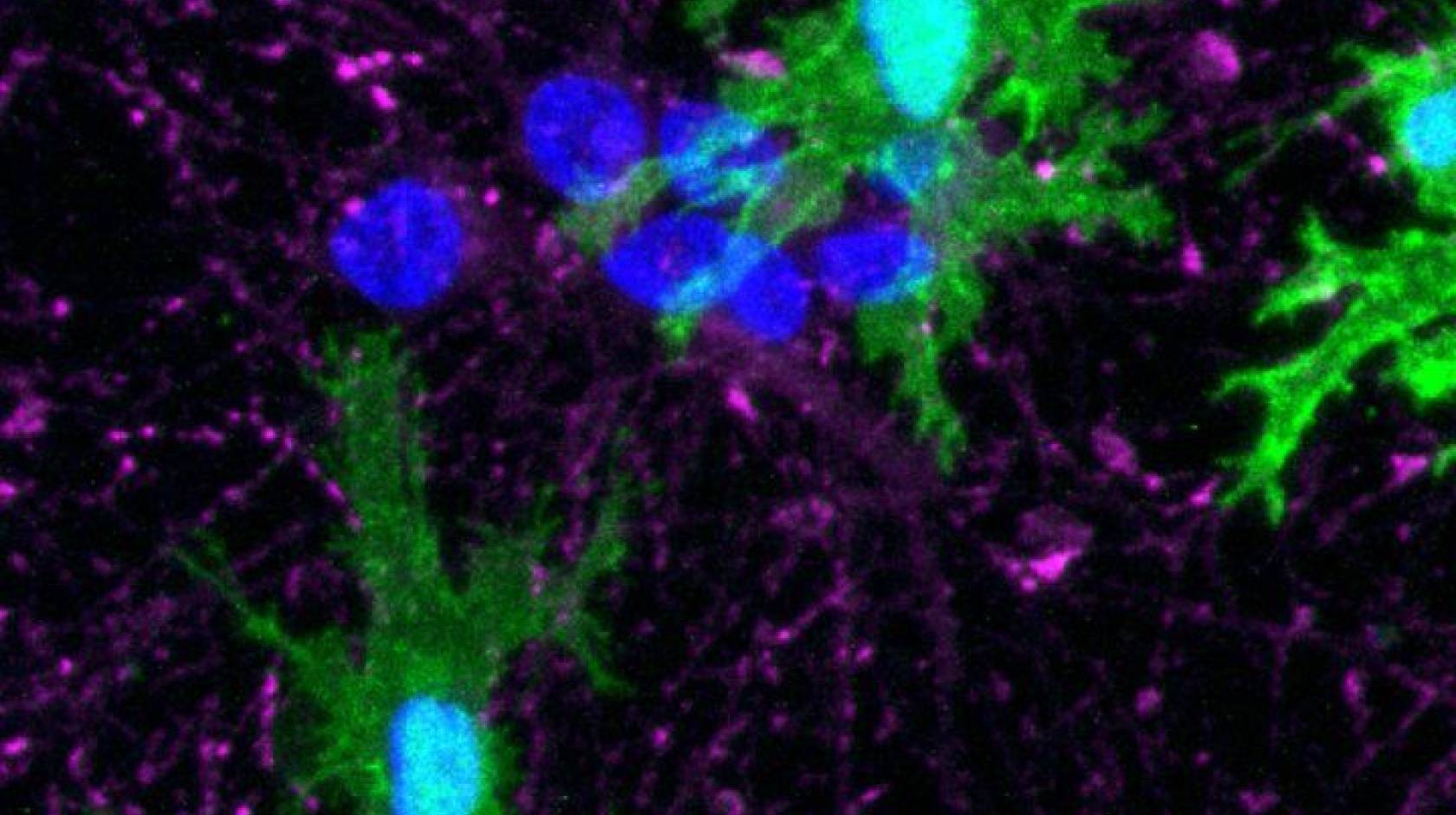
Robin Marks, UC San Francisco
The discovery of how to shift damaged brain cells from a diseased state into a healthy one presents a potential new path to treating Alzheimer’s disease and other forms of dementia, according to a new study from researchers at UC San Francisco.
The research focuses on microglia, cells that stabilize the brain by clearing out damaged neurons and the protein plaques often associated with dementia and other brain diseases.
These cells are understudied, despite the fact that changes in them are known to play a significant role Alzheimer’s and other brain diseases, said Martin Kampmann, Ph.D., senior author on the study, which appears Aug. 11 in Nature Neuroscience.
“Now, using a new CRISPR method we developed, we can uncover how to actually control these microglia, to get them to stop doing toxic things and go back to carrying out their vitally important cleaning jobs,” he said. “This capability presents the opportunity for an entirely new type of therapeutic approach.”
Leveraging the brain’s immune system
Most of the genes known to increase the risk for Alzheimer’s disease act through microglial cells. Thus, these cells have a significant impact on how such neurodegenerative diseases play out, said Kampmann, who is also part of the UCSF Weill Institute for Neurosciences.
Microglia act as the brain’s immune system. Ordinary immune cells can’t cross the blood-brain barrier, so it’s the task of healthy microglia to clear out waste and toxins, keeping neurons functioning at their best. When microglia start losing their way, the result can be brain inflammation and damage to neurons and the networks they form.
Under some conditions, for example, microglia will start removing synapses between neurons. While this is a normal part of brain development in a person’s childhood and adolescent years, it can have disastrous effects in the adult brain.
Over the past five years or so, many studies have observed and profiled these varying microglial states but haven’t been able to characterize the genetics behind them.
Kampmann and his team wanted to identify exactly which genes are involved in specific states of microglial activity, and how each of those states are regulated. With that knowledge, they could then flip genes on and off, setting wayward cells back on the right track.
From advanced genomics to a holy grail
Accomplishing that task required surmounting fundamental obstacles that have prevented researchers from controlling gene expression in these cells. For example, microglia are very resistant to the most common CRISPR technique, which involves getting the desired genetic material into the cell by using a virus to deliver it.
To overcome this, Kampmann’s team coaxed stem cells donated by human volunteers to become microglia and confirmed that these cells function like their ordinary human counterparts. The team then developed a new platform that combines a form of CRISPR, which enables researchers to turn individual genes on and off – and which Kampmann had a significant hand in developing – with readouts of data that indicate functions and states of individual microglia cells.
Through this analysis, Kampmann and his team pinpointed genes that affect the cell’s ability to survive and proliferate, how actively a cell produces inflammatory substances, and how aggressively a cell prunes synapses.
And because the scientists had determined which genes control those activities, they were able to reset the genes and flip the diseased cell to a healthy state.
Armed with this new technique, Kampmann plans to investigate how to control the relevant states of microglia, by targeting the cells with existing pharmaceutical molecules and testing them in preclinical models. He hopes to find specific molecules that act on the genes necessary to nudge diseased cells back to a healthy state.
Kampmann said that once the right genes are flipped, it’s likely that the “repaired,” microglia will resume their responsibilities, removing plaques associated with neurodegenerative disease and protecting synapses rather than taking them apart.
“Our study provides a blueprint for a new approach to treatment,” he said. “It’s a bit of a holy grail.”
Funding: This work was funded in part by NIH grants DP2 GM119139, U01 MH115747, U54 NS100717, R01 AG051390, F30 AG066418, F30 AG062043, and ZO1 AG000534-02. For other funding, please see the study
Authors: Other authors include: Nina Dräger, Sydney Sattler, Olivia M. Teter, Kun Leng, Jason Hong, Giovanni Aviles, Claire D. Clelland and Lay Kodama. Co-senior author, Li Gan formerly at UCSF, is now at Weill Cornell Medicine. For other authors, please see the study.

