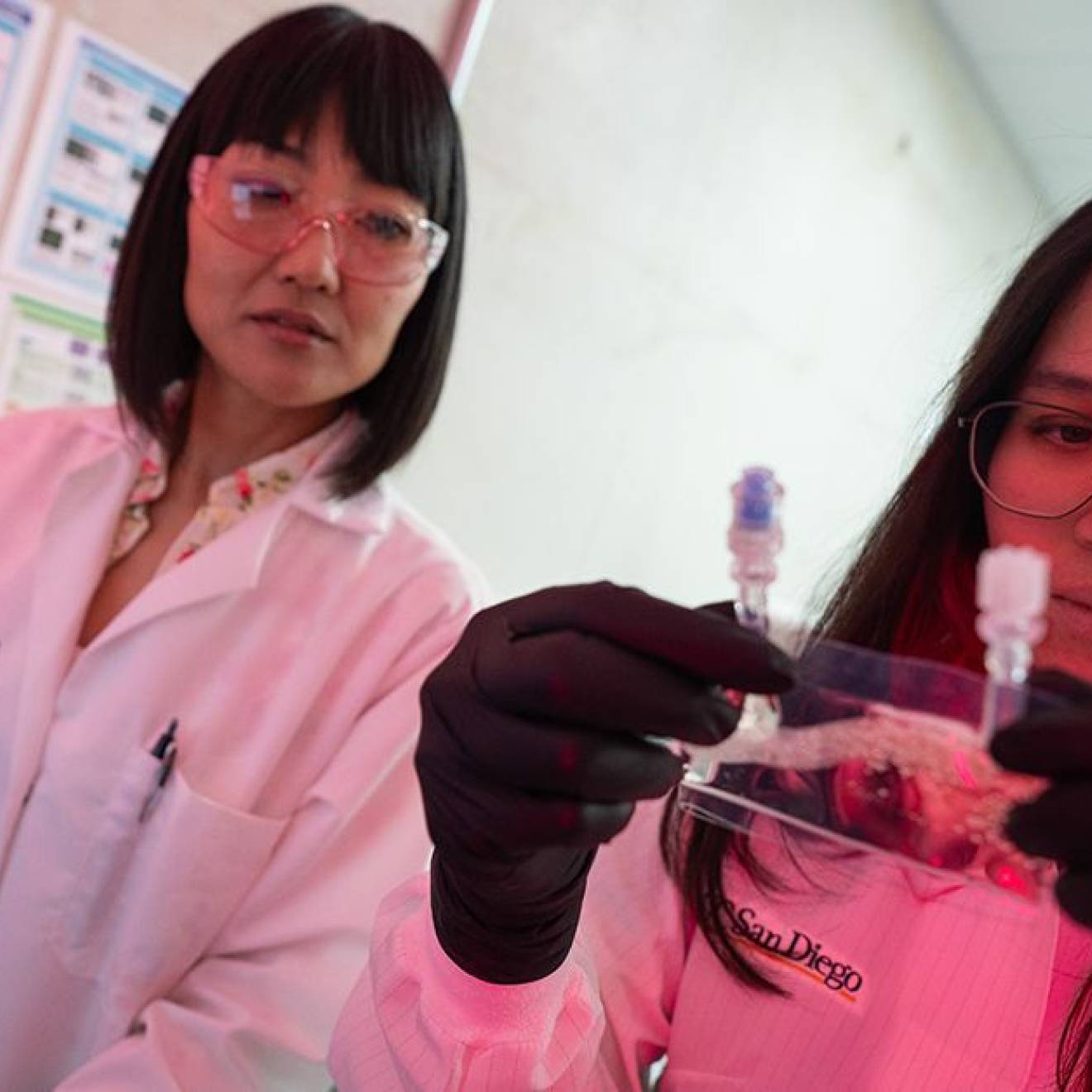
Michelle Brubaker, UC San Diego

On a July afternoon, Federico Gomez Gil, 56, is dressed in a short-sleeved, collared shirt, sweatpants and a baseball cap. He sits in a chair in a hospital room, surrounded by his wife and two daughters. Given the past five months, this is the moment of a lifetime — a new lifetime.
Gomez Gil is recovering from a double lung transplant at UC San Diego Health after a severe case of COVID-19 ravaged his body and resulted in pneumonia that permanently impaired his ability to breathe.
“I felt extremely weak. I had a fever and chills,” said Gomez Gil, an Escondido resident diagnosed with COVID-19 in February 2021, before the vaccination was available to him. “I did not feel well at all.”
As his initial condition progressively worsened, he was transferred to the Sulpizio Cardiovascular Center at UC San Diego Health. He required life-saving support and care.
“What was eye-opening was that besides the COVID-19 virus, Mr. Gomez Gil was an otherwise healthy man,” said Eugene Golts, M.D., cardiothoracic surgeon at UC San Diego Health who performed the nearly eight-hour double lung transplant surgery.
First, Gomez Gil was placed on a ventilator to assist with breathing, but it quickly became evident that a higher level of care was needed.
“He was on the brink of death when he arrived,” said Travis Pollema, D.O., a cardiothoracic surgeon at UC San Diego Health who assisted Golts. “He would not have survived if he had not come to UC San Diego Health. We were able to provide him care with a combination of advanced technologies and approaches not available at any other hospital system in San Diego.”

Credit: UC San Diego Health
Gomez Gil was placed on extracorporeal membrane oxygenation, or ECMO. It is used when a ventilator alone is insufficient. ECMO works outside the body, pumping and oxygenating a patient’s blood. The patient is connected to an ECMO machine via tubes, typically inserted into large arteries or veins in the neck and groin by cardiothoracic surgeons like Pollema. With their workload reduced, the patient’s heart and lungs are able to rest and heal.
Gomez Gil was on ECMO for more than 50 days. Prior to the pandemic, the standard time for a patient to be on ECMO was 9 to 12 days.
But ECMO is not a permanent remedy. And as the days passed, it became clear that Gomez Gil would require some form of ventilation for the rest of his life. The solution was a double lung transplant. That’s when a multi-disciplinary team of physical therapists, respiratory therapists, pulmonologists, surgeons and nursing staff began working around-the-clock to get him strong enough to be a viable candidate for the transplant surgery, which remains relatively rare. COVID-19 added a new and unknown factor.
“A requirement for transplant is that patients have a degree of mobility, even if on life support. We slowly wake patients up for periods of time and work with them to undergo a degree of physical therapy. It’s a marker for how well the patient will do following the surgery,” said Pollema.
While on ECMO, Gomez Gil did physical therapy for approximately nine weeks before his transplant surgery.
“This process can be difficult. The patient’s lungs have not worked on their own for a long period of time,” said Pollema. “With the help of a phenomenal team, we were able to work through that transition period with Mr. Gomez Gil.”
On June 14, 2021, Gomez Gil received his new lungs.
“The surgery went well and he has a good prognosis,” said Golts. “He has a long road to recovery, longer than most lung transplant patients because he needs to learn how to breathe again on his own after having mechanical lungs do it for him for so long.”
Approximately three months after surgery, Gomez Gil was discharged.
“This has been a rollercoaster of emotions,” said Guadalupe Gomez, Federico’s eldest daughter. “It has been amazing to see his progress. One day he had all these tubes in, and then eventually, they were removed and he was communicating with us. Now, he is back home. It’s been surreal.”
“I feel so much better today. I am most looking forward to spending time with my four grandkids,” said Gomez Gil. “I am so grateful to the donor and the entire medical team. I am so blessed to be a success story. I want people to know this virus is real and serious. It’s so important for everyone to protect themselves, follow all the safety precautions and get vaccinated.”
Gomez Gil’s story is an example of the premiere lung transplant program and collaboration of teams at UC San Diego Health, said Kamyar Afshar, D.O., medical director of the lung transplant program at UC San Diego Health.
“We take treating every patient as an individual seriously. We want them to be able to enjoy their life with their loved ones for many years,” Afshar said. “We take great pride to have been part of Mr. Gomez Gil’s medical team. It is incredible to witness what we as people can overcome. We were able to nurse a gravely ill patient to the point of transplant and then give him a second chance at life.”

Credit: UC San Diego Health
Post-transplant care for Gomez Gil includes strict monitoring from his medical team, daily anti-rejection and anti-infection medications, exercise and physical rehabilitation.
UC San Diego Health is the only hospital system in San Diego that performs lung transplants. The program is ranked No. 1 in the nation for one-year patient survival rates among programs with a volume of 50 to 75 lung transplants performed, and No. 3 among all lung transplant programs. It is part of a Pulmonary and Critical Care specialty ranked among the best in the nation by U.S. News & World Report. Recently, the ECMO program at UC San Diego Health received the Extracorporeal Life Support Organization (ELSO) Gold Level Center of Excellence award.