Heather Buschman, Ph.D. and Jeanna Vazquez, UC San Diego
There are no Food and Drug Administration (FDA)-approved treatments for COVID-19, the pandemic infection caused by a novel coronavirus. While several therapies are being tested in clinical trials, current standard of care involves providing patients with fluids and fever-reducing medications. To speed the search for new COVID-19 therapies, researchers are testing repurposed drugs — medicines already known to be safe for human use because they are FDA-approved for other conditions — for their abilities to mitigate the virus.
UC San Diego Health researchers recently reported that statins — widely used cholesterol-lowering medications — are associated with reduced risk of developing severe COVID-19 disease, as well as faster recovery times. A second research team at UC San Diego School of Medicine has uncovered evidence that helps explains why: In short, removing cholesterol from cell membranes prevents the coronavirus from getting in.
The clinical study, published September 15, 2020 in American Journal of Cardiology, was led by Lori Daniels, M.D., professor and director of the Cardiovascular Intensive Care Unit at UC San Diego Health, and Karen Messer, Ph.D., professor and chief of the Division of Biostatics and Bioinformatics in the Department of Family Medicine and Public Health.
The mechanistic study, published September 18, 2020 in The EMBO Journal, was led by Tariq Rana, Ph.D., professor and chief of the Division of Genetics in the Department of Pediatrics at UC San Diego School of Medicine and Moores Cancer Center.
Patients with COVID-19 who took statins fared better
A molecule known as ACE2 sits like a doorknob on the outer surfaces of many human cells, where it helps regulate and lower blood pressure. ACE2 can be affected by prescription statins and other medications used for cardiovascular disease.
But, in January 2020, researchers discovered a new role for ACE2: SARS-CoV-2, the coronavirus that causes COVID-19, primarily uses the receptor to enter lung cells and establish respiratory infections.
“When faced with this novel virus at the beginning of the pandemic, there was a lot of speculation surrounding certain medications that affect ACE2, including statins, and if they may influence COVID-19 risk,” Daniels said. “We needed to confirm whether or not the use of statins has an impact on a person’s severity of SARS-CoV-2 infection and determine if it was safe for our patients to continue with their medications.”
To do this, Daniels, Messer and team retrospectively analyzed the electronic medical records of 170 patients with COVID-19 and 5,281 COVID-negative control patients hospitalized at UC San Diego Health between February and June 2020. They collected anonymized data that included the patients’ disease severity, length of hospital stay, outcome, and use of statins, angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) within 30 days prior to hospital admission.

Credit: UC San Diego
Among the patients with COVID-19, 27 percent were actively taking statins on admission, while 21 percent were on an ACE inhibitor and 12 percent on an ARB. The median length of hospital stay was 9.7 days for patients with COVID-19.
The researchers found that statin use prior to hospital admission for COVID-19 was associated with a more than 50 percent reduction in risk of developing severe COVID-19, compared to those with COVID-19 but not taking statins. Patients with COVID-19 who were taking statins prior to hospitalization also recovered faster than those not taking the cholesterol-lowering medication.
“We found that statins are not only safe but potentially protective against a severe COVID-19 infection,” said Daniels. “Statins specifically may inhibit SARS-CoV-2 infection through its known anti-inflammatory effects and binding capabilities as that could potentially stop progression of the virus.”
This initial study was relatively small and focused on a single health system. Moving forward, Daniels is partnering with the American Heart Association to analyze thousands of patients all over the country to corroborate the data she’s developed locally.
“I tell my patients who are on statins, ACE inhibitors or other ARBs to keep taking them,” she said. “Fears of COVID-19 should not be a reason to stop, if anything our research findings should be incentive to continue with their medication.”
Draining cholesterol from cell membranes blocks SARS-CoV-2 entry
Statins weren’t yet on Rana’s radar when they began their EMBO Journal study approximately six months ago. At first, his team was simply curious to see which genes are switched “on” in human lung cells in response to SARS-CoV-2 infection.
A gene called CH25H was “blazing hot,” Rana said. CH25H encodes an enzyme that modifies cholesterol. “I got excited because with HIV, Zika, and a few others, we know that CH25H blocks the virus’ ability to enter human cells.”
Here’s what’s happening inside our cells: CH25H’s enzymatic activity produces a modified form of cholesterol called 25-hydroxycholesterol (25HC). In turn, 25HC activates another enzyme called ACAT, found inside cells in the endoplasmic reticulum. ACAT then depletes accessible cholesterol on the cell’s membrane. It’s a normally occurring process that gets kicked into high gear during some viral infections.
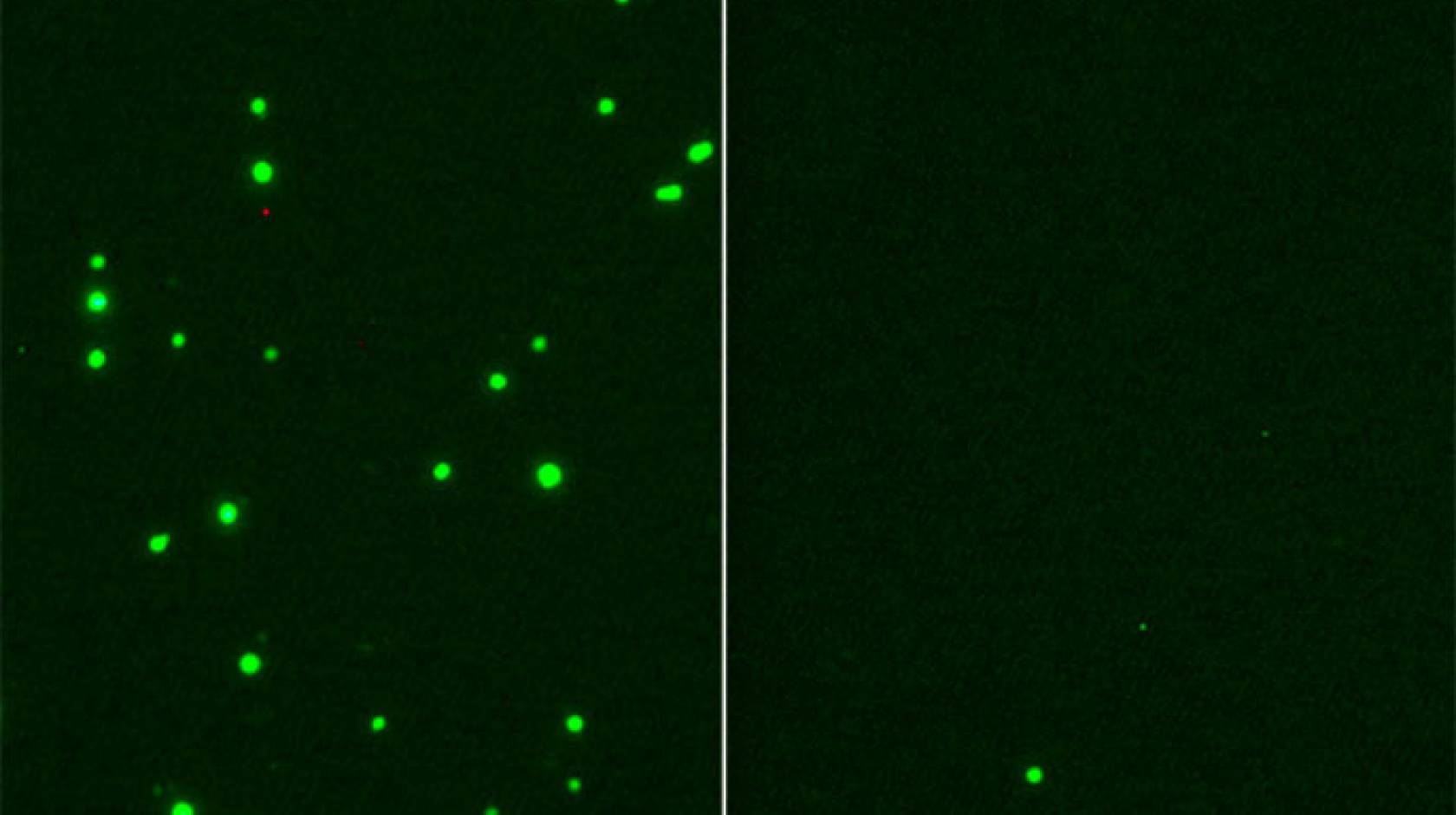
The team quickly got to work examining 25HC in the context of SARS-CoV-2 from several angles. They explored what happens to human lung cells in the lab with and without 25HC treatment when they are exposed to first a noninfectious virus that carries the SARS-CoV-2 spike protein (its key to cell entry) or to live SARS-CoV-2 virus itself.
No matter which way they came at it, added 25HC inhibited the ability of the virus to enter cells — blocking infection almost completely.
“The difference between untreated cells and those treated with 25HC was like day and night,” Rana said.
While SARS-CoV-2 uses the ACE2 receptor to initially dock on a cell, Rana’s study suggests that the virus also needs cholesterol (normally found in cell membranes) in order to fuse with and enter the cell. 25HC takes away a lot of that membrane cholesterol, preventing viral entry.
In a similar way, statins are likely beneficial in preventing or reducing the severity of SARS-CoV-2 infection because, while intended to remove cholesterol from blood vessels, they are also removing cholesterol from cell membranes. As a result, the coronavirus can’t get in.
“This is already happening in our bodies on a regular basis, so perhaps we just need to give it a boost, with statins or by other means, to better resist some viruses,” Rana said. “It’s not unlike cancer immunotherapy — the idea that sometimes instead of attacking a tumor directly, it’s better to arm a patient’s immune system to do a better job of clearing away tumors on its own.”
If it can be developed into a therapeutic, 25HC might work even better as an antiviral than statins, Rana said. That’s because it works specifically on cholesterol in cell membranes, rather than cholesterol throughout the body. Like all medications, statins can cause negative side effects, including digestive problems and muscle pains, and may not be an option for many people with COVID-19. What’s more, while some previous studies suggested statins may also elevate ACE2 levels, which could allow more viral entry, Rana’s team did not see an increase in the receptor in response to 25HC.
Statins are FDA-approved for human use, but 25HC is a natural product currently available only for laboratory work. Rana and team plan to continue optimizing 25HC as a potential antiviral agent. Many steps remain before it might be tested in human clinical trials.
Co-authors of the American Journal of Cardiology study also include: Christopher Longhurst, Amy Sitapati, Jing Zhang, Jingjing Zou, Quan Bui, Junting Ren, Michael Criqui, all at UC San Diego.
Funding for this research came, in part, from the University of California Office of the President (grant R00RG24990).
Co-authors of The EMBO Journal study also include: Shaobo Wang, Wanyu Li, Hui Hui, Shashi Kant Tiwari, Qiong Zhang, Ben A. Croker, Stephen Rawlings, Davey Smith and Aaron F. Carlin, all at UC San Diego.
Funding for this research came, in part, from National Institutes of Health (grants CA177322, DA039562, DA049524 and AI125103), Burroughs Wellcome Fund and John and Mary Tu Foundation.
Disclosure: Tariq Rana is a founder of ViRx Pharmaceuticals and has an equity interest in the company. The terms of this arrangement have been reviewed and approved by the University of California San Diego in accordance with its conflict of interest policies.

