Nicholas Weiler, UCSF
Using video microscopy in the living mouse lung, UC San Francisco scientists have revealed that the lungs play a previously unrecognized role in blood production. As reported online March 22, 2017, in Nature, the researchers found that the lungs produced more than half of the platelets — blood components required for the clotting that stanches bleeding — in the mouse circulation.
In another surprise finding, the scientists also identified a previously unknown pool of blood stem cells capable of restoring blood production when the stem cells of the bone marrow, previously thought to be the principal site of blood production, are depleted.

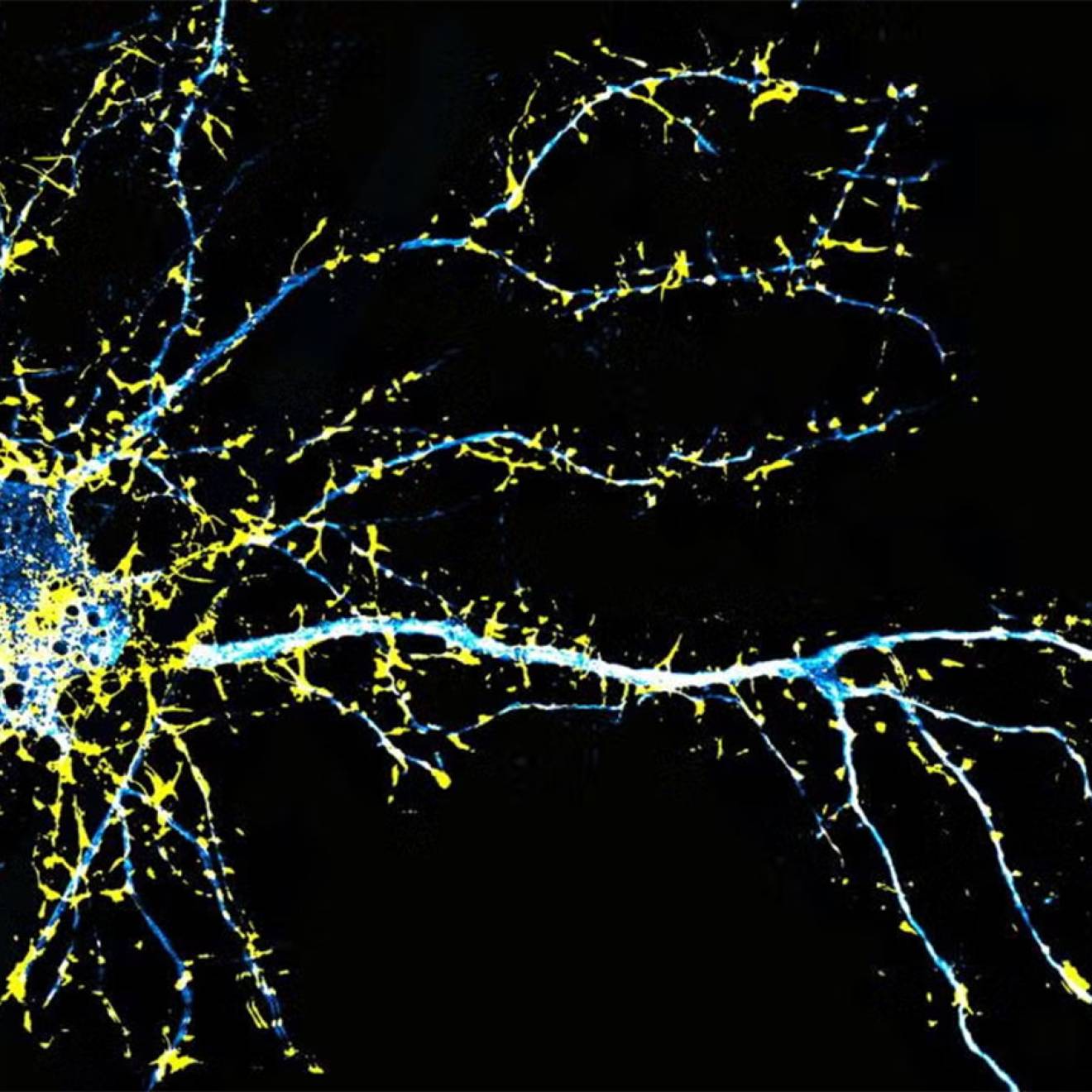
Credit: UCSF
“This finding definitely suggests a more sophisticated view of the lungs – that they’re not just for respiration but also a key partner in formation of crucial aspects of the blood,” said pulmonologist Mark R. Looney, a professor of medicine and of laboratory medicine at UCSF and the new paper’s senior author. “What we’ve observed here in mice strongly suggests the lung may play a key role in blood formation in humans as well.”
The findings could have major implications for understanding human diseases in which patients suffer from low platelet counts, or thrombocytopenia, which afflicts millions of people and increases the risk of dangerous uncontrolled bleeding. The findings also raise questions about how blood stem cells residing in the lungs may affect the recipients of lung transplants.
Lungs produce more than 10 million platelets per hour
The new study was made possible by a refinement of a technique known as two-photon intravital imaging recently developed by Looney and co-author Matthew F. Krummel, a UCSF professor of pathology. This imaging approach allowed the researchers to perform the extremely delicate task of visualizing the behavior of individual cells within the tiny blood vessels of a living mouse lung.

Credit: UCSF
Looney and his team were using this technique to examine interactions between the immune system and circulating platelets in the lungs, using a mouse strain engineered so that platelets emit bright green fluorescence, when they noticed a surprisingly large population of platelet-producing cells called megakaryocytes in the lung vasculature. Though megakaryocytes had been observed in the lung before, they were generally thought to live and produce platelets primarily in the bone marrow.
“When we discovered this massive population of megakaryocytes that appeared to be living in the lung, we realized we had to follow this up,” said Emma Lefrançais, a postdoctoral researcher in Looney’s lab and co-first author on the new paper.
More detailed imaging sessions soon revealed megakaryocytes in the act of producing more than 10 million platelets per hour within the lung vasculature, suggesting that more than half of a mouse’s total platelet production occurs in the lung, not the bone marrow, as researchers had long presumed. Video microscopy experiments also revealed a wide variety of previously overlooked megakaryocyte progenitor cells and blood stem cells sitting quietly outside the lung vasculature — estimated at 1 million per mouse lung.
Blood stem cells in the lung can restore bone marrow
The discovery of megakaryocytes and blood stem cells in the lung raised questions about how these cells move back and forth between the lung and bone marrow. To address these questions, the researchers conducted a clever set of lung transplant studies:
First, the team transplanted lungs from normal donor mice into recipient mice with fluorescent megakaryocytes, and found that fluorescent megakaryocytes from the recipient mice soon began turning up in the lung vasculature. This suggested that the platelet-producing megakaryocytes in the lung originate in the bone marrow.
“It’s fascinating that megakaryocytes travel all the way from the bone marrow to the lungs to produce platelets,” said Guadalupe Ortiz-Muñoz, a postdoctoral researcher in the Looney lab and the paper’s other co-first author. “It’s possible that the lung is an ideal bioreactor for platelet production because of the mechanical force of the blood, or perhaps because of some molecular signaling we don’t yet know about.”
"It’s possible that the lung is an ideal bioreactor for platelet production because of the mechanical force of the blood, or perhaps because of some molecular signaling we don’t yet know about."
–Guadalupe Ortiz-Muñoz, postdoctoral researcher in the Mark Looney Lab
In another experiment, the researchers transplanted lungs with fluorescent megakaryocyte progenitor cells into mutant mice with low platelet counts. The transplants produced a large burst of fluorescent platelets that quickly restored normal levels, an effect that persisted over several months of observation — much longer than the lifespan of individual megakaryocytes or platelets. To the researchers, this indicated that resident megakaryocyte progenitor cells in the transplanted lungs had become activated by the recipient mouse’s low platelet counts and had produced healthy new megakaryocyte cells to restore proper platelet production.
Finally, the researchers transplanted healthy lungs in which all cells were fluorescently tagged into mutant mice whose bone marrow lacked normal blood stem cells. Analysis of the bone marrow of recipient mice showed that fluorescent cells originating from the transplanted lungs soon traveled to the damaged bone marrow and contributed to the production not just of platelets, but of a wide variety of blood cells, including immune cells such as neutrophils, B cells and T cells. These experiments suggest that the lungs play host to a wide variety of blood progenitor cells and stem cells capable of restocking damaged bone marrow and restoring production of many components of the blood.
“To our knowledge this is the first description of blood progenitors resident in the lung, and it raises a lot of questions with clinical relevance for the millions of people who suffer from thrombocytopenia,” said Looney, who is also an attending physician on UCSF’s pulmonary consult service and intensive care units.
Lungs as resource for platelet production
In particular, the study suggests that researchers who have proposed treating platelet diseases with platelets produced from engineered megakaryocytes should look to the lungs as a resource for platelet production, Looney said. The study also presents new avenues of research for stem cell biologists to explore how the bone marrow and lung collaborate to produce a healthy blood system through the mutual exchange of stem cells.
“These observations alter existing paradigms regarding blood cell formation, lung biology and disease, and transplantation,” said pulmonologist Guy A. Zimmerman, who is associate chair of the Department of Internal Medicine at the University of Utah School of Medicine and was an independent reviewer of the new study for Nature. “The findings have direct clinical relevance and provide a rich group of questions for future studies of platelet genesis and megakaryocyte function in lung inflammation and other inflammatory conditions, bleeding and thrombotic disorders, and transplantation.”
The observation that blood stem cells and progenitors seem to travel back and forth freely between the lung and bone marrow lends support to a growing sense among researchers that stem cells may be much more active than previously appreciated, Looney said. “We’re seeing more and more that the stem cells that produce the blood don’t just live in one place but travel around through the blood stream. Perhaps ‘studying abroad’ in different organs is a normal part of stem cell education.”
The study was supported the UCSF Nina Ireland Program in Lung Health, the UCSF Program for Breakthrough Biomedical Research, and the National Heart, Lung, and Blood Institute (NHLBI), a division of the National Institutes of Health (HL092471, HL107386 and HL130324).
“It has been known for decades that the lung can be a site of platelet production, but this study amplifies this idea by demonstrating that the murine lung is a major participant in the process,” said Traci Mondoro, project officer at the Translational Blood Science and Resources Branch of the NHLBI. “Dr. Looney and his team have disrupted some traditional ideas about the pulmonary role in platelet-related hematopoiesis, paving the way for further scientific exploration of this integrated biology.”
Additional authors included Axelle Caudrillier, Beñat Mallavia, Fengchun Liu, Emily E. Thornton, Mark B. Headley, Tovo David, Shaun R. Coughlin, Andrew D. Leavitt, David M. Sayah, of UCLA; and Emmanuelle Passegué, a former UCSF faculty member who is now director of the Columbia Stem Cell Initiative at Columbia University Medical Center.
Cover photo: iStock/choja