Alison Caldwell, UC San Diego
Even as university campuses close across the nation in an effort to slow the spread of the novel coronavirus, a team of engineers and physicians at the University of California, San Diego is rapidly developing simple, ready-to-use ventilators to be deployed if the need arises.
The project kick-started several weeks ago when news started to trickle in that communities in Northern Italy with widespread COVID-19 were in dire straits.
“One of the biggest things we heard was that there weren’t enough ventilators to treat all of the patients coming into the hospitals,” said James Friend, a professor in the Department of Mechanical and Aerospace Engineering and the Department of Surgery at UC San Diego. “It’s clear that if we’re not careful, we might end up in the same situation.”
Credit: UC San Diego
Ventilators are medical devices that push air in and out of a patient’s lungs when they are unable to breathe on their own. One of the primary symptoms of COVID-19 is difficulty in breathing; approximately 1 percent of people who contract the virus require ventilation to support their recovery — sometimes for weeks.
The situation in Italy spurred Dr. Lonnie Petersen, an assistant professor in the Department of Mechanical and Aerospace Engineering at UC San Diego and an adjunct with UC San Diego Health, to reach out to her medical and engineering colleagues, proposing a new collaboration to quickly produce simple ventilators that could be easily built and readily used to support patients in a crisis.
“We immediately had a lot of support from staff and faculty, all working to get this project off the ground,” Petersen said. “Our community is taking this threat very seriously and acting accordingly.”
The first step was to seek consensus with anesthetists and respiratory therapists about minimum requirements for a ventilator. The next was to determine whether engineers could reasonably produce them, and how quickly.
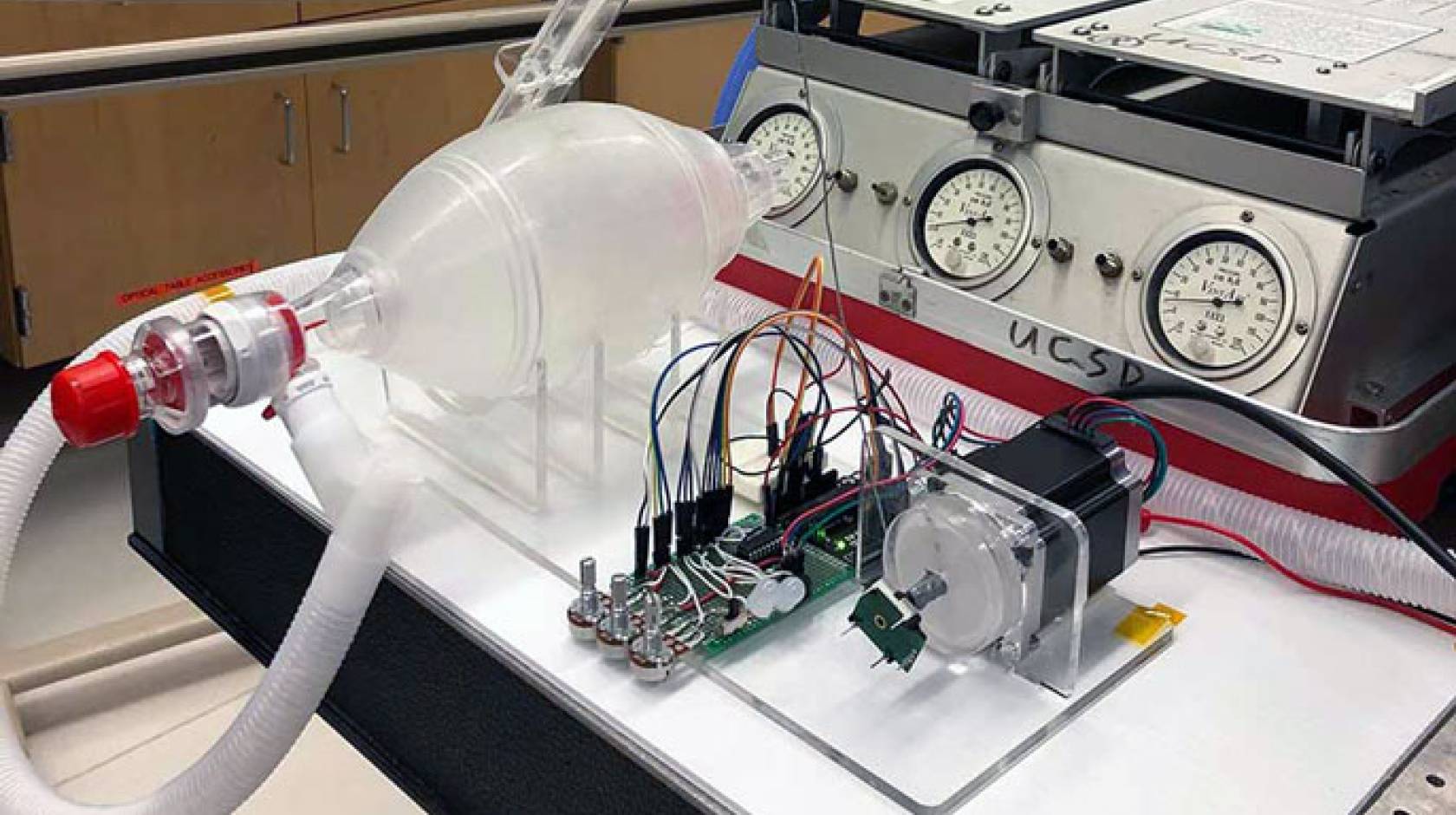
Within days, a team of researchers from the Friend and Petersen labs, including graduate students Aditya Vasan, William Connacher, Jeremy Sieker and Reiley Weekes, began building devices using premade parts and 3-D printers. Their first goal was to convert an existing manual ventilator model to automatic, able to provide breathing assistance without human intervention.
The existing manual design features a mask fitted over a patient’s face and a bag that can be squeezed by hand to push air into the patient’s lungs. The team is designing a machine that can do the squeezing instead, freeing doctors and nurses to address other concerns.
“We’re 3-D printing parts that can be attached to a motor to compress the bag of the manual ventilator,” said Ph.D. student Vasan. “This allows us to control the speed and volume of the compressions to help patients breathe.”
The advantage of 3-D printing is that it can be used to quickly produce customized parts. Devices can be made on a small scale much faster than by traditional manufacturing methods.
“As long as the correct materials are used, 3-D printing can be used to produce a wide variety of tools in the fight against COVID-19,” said Shaochen Chen, a professor of nanoengineering at the Jacobs School of Engineering. “It’s not good for, say, entire N-95 masks, but it can be used for producing testing swabs or even face shields for healthcare workers.”
Meanwhile, Petersen’s team is awaiting a few more parts to build a more sophisticated ventilator using an electric pump. “Our aim is to have functional devices as soon as possible,” she said. “Once we’ve got the bare bones system up and running, we can start adding layers of sophistication and automation. Those additional layers will include advanced regulation of air pressure and flow to allow for a more disease-specific and patient-tailored respiratory support.”
The first ventilators will be simple, but the goal is to have something readily at hand when the need arises.
But a simple design isn’t the team’s only goal.
A broader goal and volunteers needed
“We are preparing for a shortage of both ventilators and specialized staff to run them,” said Petersen. “The questions quickly became ‘How can we tweak the ventilators that are available to support multiple patients? How can we create more ventilators that are easier for staff to use?’”
Other projects include collecting and inventorying oxygen supplies in preparation for increased demand by local hospitals; converting other air pressure machines, such as CPAPs and Bi-PAPs into ventilators; and adapting existing ventilators to serve more patients.

Credit: UC San Diego
The team hopes to have functional prototypes within a few days and are ready to test them in simulators, in collaboration with anesthesiologists, before potentially applying to patients.
“Normally, the production timeline on something like this would be months, or even years,” said Petersen. “By building on existing technology and taking multiple steps at once, we aim to reduce that timeline to weeks.”
While grappling with challenges in locating parts that can’t be 3-D printed and obtaining them from outside vendors, the biggest roadblock right now is gathering enough people to assemble the devices.
The UC San Diego campus is largely closed and empty, due to efforts to minimize coronavirus exposure and slow the spread of COVID-19. The graduate student team continues work, thanks to a special exception granted by the Dean of the Jacobs School of Engineering.
“This is a team effort,” said Petersen. “And we can use the assistance of other engineers. We would love to hear from students, staff, and faculty with hands-on engineering experience who can help us with this project.”
Qualified volunteers should email: UCSDVentilatorEngHelp@gmail.com
Splitting ventilators
Meanwhile, Petersen’s colleague Dr. Sidney Merritt, an associate clinical professor of anesthesiology at UC San Diego Health, is working with a team that includes U.S. Navy and Lockheed Martin personnel to develop a 3-D-printable system for splitting a ventilator designed for one patient so that it can be used by up to four patients at a time.
“We found a file online that showed us how it could be done,” said Merritt. “We’ve been working with the Navy and others to print them in different materials and test them on a ventilator, and, so far, it works. We were able to get enough pressure on each line that it should be adequate for serving four patients at a time.”
The challenge now is finding valves that can regulate the pressure for each patient on the system and monitor individual air pressure for each one, allowing for the fine control needed to support each patient’s specific needs. “As soon as we have the valves worked out, we’ll be just a couple days out from getting them set up and running,” said Merritt.

Credit: UC San Diego
“This situation is going to be very severe,” she continued. “We need to have every tool available to us, so we are ready to treat patients because we still don’t know how many people will get sick.”
Despite obstacles, the team said it has been overwhelmed by support and advocacy from colleagues and university leadership. For example, the Institute on Global Conflict and Cooperation at UC San Diego has contributed $50,000 to assist in the development of prototypes.
“The UC San Diego family is really pulling together on this one,” said Petersen. “From the dean, through chairs, faculty and students, regardless of who we’ve spoken to, everyone has gone above and beyond to help with this project as much as they can. It’s really bringing the community together. Everyone is moving in the same direction. While the work may be preparing for something unpleasant, it’s very good to be working in such a supportive environment.”
Other members of the continuously growing team include Dr. Daniel Lee; Dr. Preetham Suresh; Dr. William Mazzei; Dr. Matthew Follansbee; Dr. Micheal Vanietti; Dr. Hemal Patel; Theodore Vallejos of UC San Diego Health; Mark Stambaugh of the Qualcomm Institute; and Tania Morimoto, a professor in the Department of Aerospace and Engineering at the Jacobs School.

