Julia Busiek, UC Newsroom
Adolescence would be hard enough without pimples. But in a cruel twist of biology, acne tends to strike during our teens, when many people are already at their most awkward and self-conscious.
Acne “causes mental health problems,” says George Liu, professor and chief of infectious disease in the department of pediatrics at UC San Diego. “Folks stress so much over it, and it causes social stigma.”
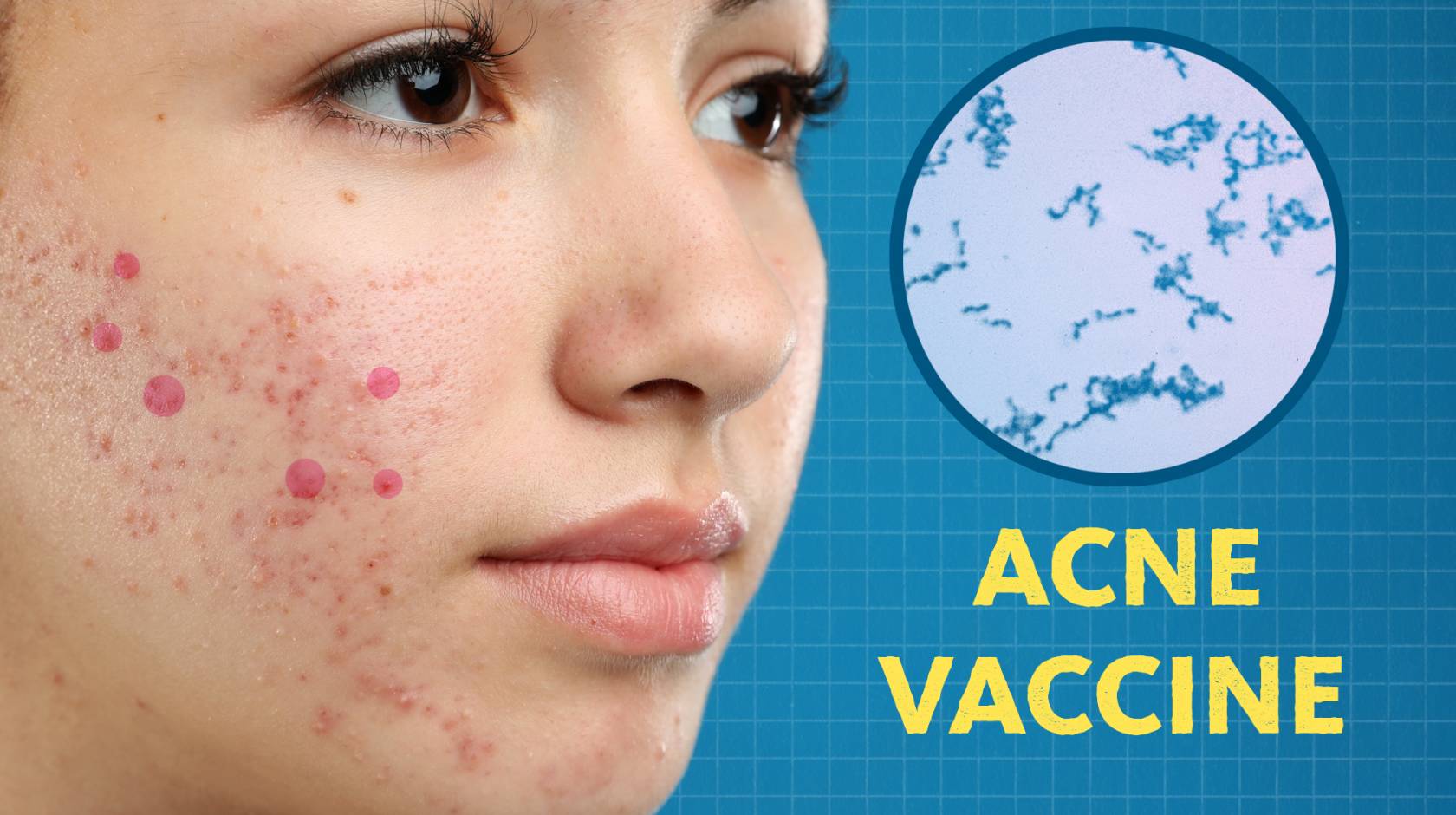
Good news for anyone who’s ever been or known a teenager: Liu’s team is getting closer to developing the first vaccine against acne.
Learn more about their quest in the latest episode of Fig. 1:
A complex condition
Even though most people — up to 85 percent of us — will get acne at some point in our lives, and contrary to what you’ll see from skincare ads, we still don’t have a great way to stop it. Milder cases might clear up on their own or with special face washes, but some people might need to start taking antibiotics. “In more severe cases, this could elevate to needing heavy gun immunosuppressants,” says Liu.
These therapies can zap the zits — but come with some gnarly side effects. You might develop an allergic reaction to sunshine, or inadvertently make your face into a breeding ground for a super-race of antibiotic-resistant bacteria.
“If you go just online anywhere, you'll find so many ways that folks are trying to improve acne treatment,” Liu says. “That shows that it is a really difficult thing to treat.”

And it’s tough to treat in part because the causes of acne are complex. We know our hormones go haywire in adolescence. That makes glands surrounding our hair follicles produce too much oil, or sebum. Some sebum is good: it keeps your skin and hair soft and protected. But make too much and the glands that produce it can get clogged and start to bulge above your skin.
That’s a pimple. Pimples are weak spots in your body’s natural defenses, where bacteria that normally lives harmlessly on your skin can get in and cause infection, inflammation and cysts.
But why do some people escape adolescence pimple free, while others suffer acne flare-ups for years?
It turns out acne is governed by a mystifying maze of interactions between your genes, diet, stress, environment, and more. Even eating chocolate might cause flare-ups in some people, Liu says.
Zooming in on the bacterial cause of acne
As an infectious disease expert, Liu’s work focuses on bacteria. His team has zeroed in on the role of one species of bacteria that scientists have long recognized is associated with the condition. The bug is named Cutibacterium acnes, since it’s commonly found on regions of skin suffering an acne outbreak.
Almost everyone’s face is home to robust C. acnes colonies. But not all cases of acne are alike. To understand why the bacteria only causes acne in some people, researchers started “picking out these bacteria directly from the acne lesion,” Liu says.
That unsettling quest turned up a clue: just as not all cases of acne are alike, neither are all colonies of C. acnes. Research turned up separate strains of the bacteria — those that are almost exclusively found inside pimples, and those that are almost always found on healthy areas of skin.
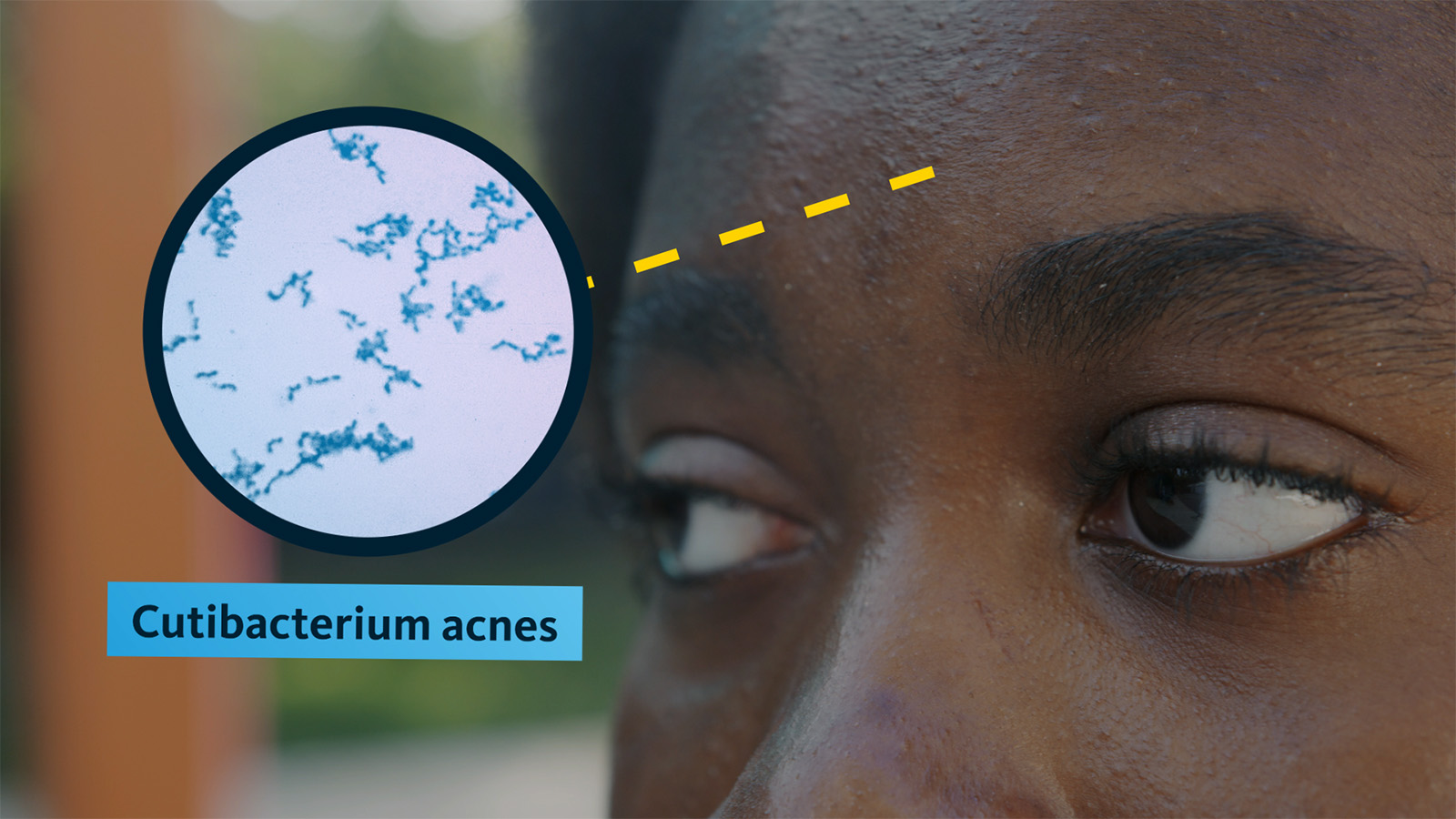
“Whatever genetic differences between these two strains, we thought they must hold the key as to what causes these lesions that are inflammatory,” he says.
To study the question, Liu’s team cooked up a batch of synthetic human sebum, smeared it on lab mice, and injected those mice with the two strains of C. acnes bacteria, which caused the mice to break out.
Studying the mice’s microbiology, Liu zeroed in on an enzyme that C. acnes bacteria produce called hyaluronidase. Hyaluronidase breaks down hyaluronic acid, a protective substance produced by your skin.
Liu’s research discovered that hyaluronidase produced by C. acnes comes in 2 flavors: Hyl-A and Hyl-B. Bacteria found inside pimples produce Hyl-A, and those found on healthy skin produced Hyl-B. Hyl-A only partially breaks down hyaluronic acid, leaving large fragments on the skin. Hyl-B, however, breaks the substance down completely.
“Why is that important? Because the larger pieces are inflammatory,” Liu says. Your immune system recognizes these large fragments as a “an alert, a danger signal that you may need to protect your body from some type of attack.” So it floods the area with heat, white blood cells and other defense mechanisms, causing inflammation.
The Hyl-B form of the enzyme, meanwhile, actually lessened acne by breaking hyaluronic acid down to much smaller molecules. These smaller molecules bind to the same receptors in your skin that the larger molecules do. That matters for two reasons: first, the smaller molecules block the larger ones from binding and provoking inflammation, and next, your immune system doesn’t recognize the smaller molecules as a threat, so it doesn’t respond with an immune attack.
This could benefit the strain of bacteria that produce the acne-fighting Hyl-B enzyme, possibly allowing them to fly under the immune system’s radar, rather than being attacked by an inflammation response that’s designed to kill the bacteria off. “Bacteria always have a last laugh,” Liu says.
Testing out vaccines
With this discovery in hand, Liu’s team compared the microscopic structures of the two different enzymes, and identified the tiny section in the bacteria’s genome that produces the enzyme.
With that, they tested a few different formulas of vaccines that targeted C. acnes. The first draft was designed to fight all types of C. acnes bacteria. In mice that had been injected only with the strain of bacteria that produced Hyl-A, which causes acne, that vaccine made the acne much better. But in mice that were host to the strain of C. acnes associated with clear skin, this vaccine actually made their acne worse, because it got rid of the hyaluronidase enzyme that had been counteracting inflammation.
“So we went back to the drawing board and concocted a vaccine that strictly attacks the Hyl-A and not the Hyl-B,” Liu says.
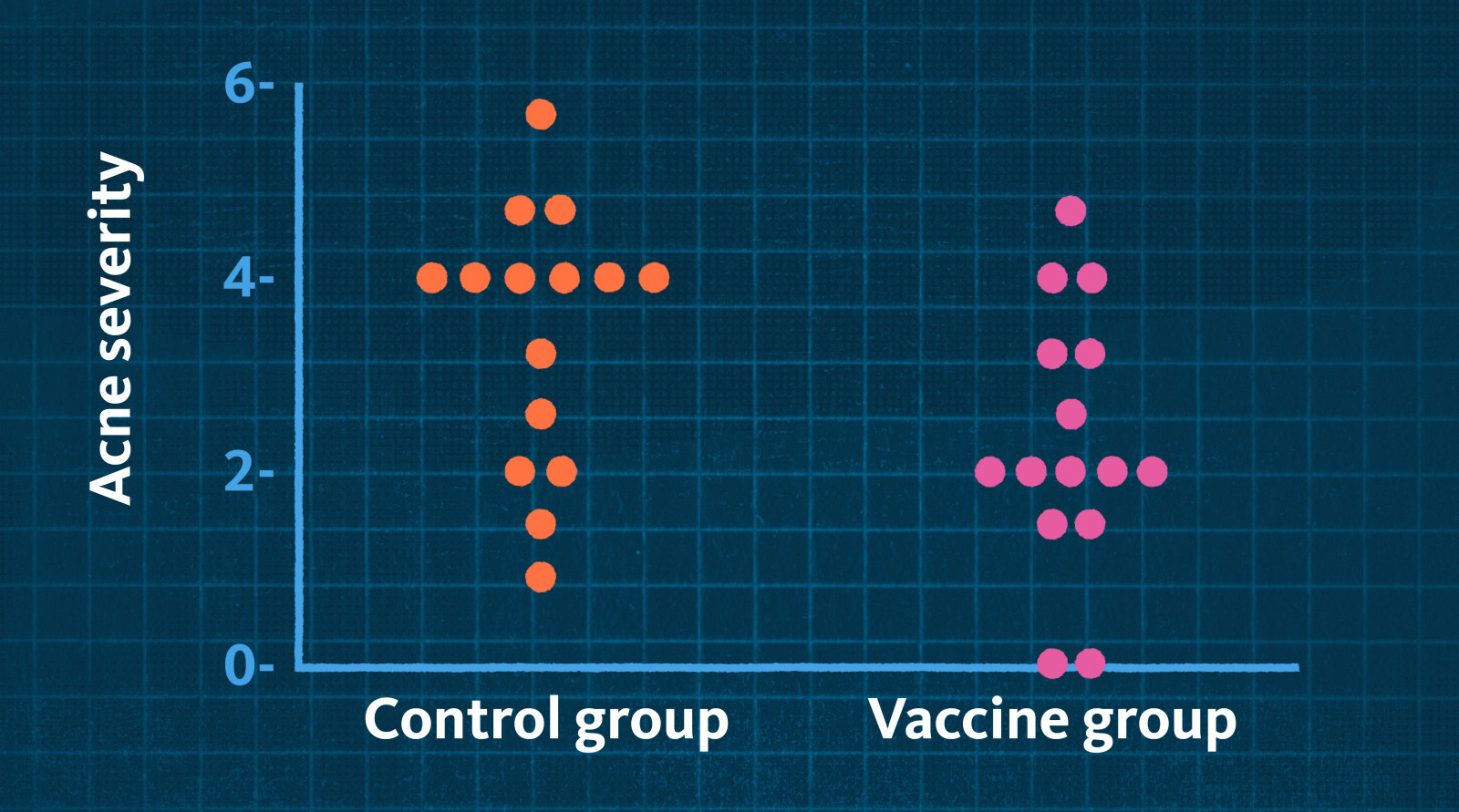
The second draft alleviated acne in the mice with the acne-causing, Hyl-A-producing bacteria, and didn’t make matters worse for mice with the acne-preventing, Hyl-B-producing bacteria. Early tests showed this form of the vaccine reduced acne severity by half.
What’s next for acne patients?
It’s a promising result, but Liu says it’s probably too soon to toss your Acutane out with the bathwater. “We have what we think is a major component of what drives acne severity from the bacteria. But do I expect targeting hyaluronidase to take away all acne? No, I don’t,” he says.
He and his colleagues are already working on ways to study human genetics and environmental factors that cause acne. It’s just a part of his portfolio, but at least some people in his orbit share his view that it’s incredibly important.
“I do other types of bacterial research, like research on Staphylococcus aureus which causes serious infections, where a vaccine is lifesaving,” Liu says. “When I talk to my teenage nephews and nieces about staph research, they don’t appear interested. But when I tell them about the acne vaccine, they’re all ears.”