Nicholas Weiler and Jim Oldfield, UCSF
Researchers at the University of Toronto and UC San Francisco have discovered that the intestine is the source of immune cells that reduce brain inflammation in people with multiple sclerosis (MS), and that increasing the number of these cells blocks inflammation entirely in a preclinical model of the disease.

Credit: Jim Oldfield/University of Toronto.
The cells in question are plasma cells — white blood cells that originate as B cells in the bone marrow but change their behavior when triggered by microbes in the gut. Studying mice and samples from human MS patients, the researchers found that plasma cells that reside in the gut and produce Immunoglobulin A (IgA) antibodies appear to migrate to the central nervous system and produce an anti-inflammatory effect during MS flare-ups.
MS is an autoimmune disease, driven by other types of immune cells (including B and T cells) that attack myelin, the protective coating that surrounds nerve fibers. Recent clinical studies have shown drugs that target B cells mitigate MS, while those that target plasma cells make the disease worse. The current study offers an explanation for these divergent results.
“We already knew what was and was not working in the clinic,” said Jen Gommerman, Ph.D., a professor of immunology at the University of Toronto and the senior author on the study. “But here we’ve uncovered the molecular and cellular mechanism at play. It’s a kind of reverse translation approach, which highlights the importance of the gut-brain axis in MS and other autoimmune conditions.”
The results were published online Jan. 3, 2019, in Cell.
The first step toward producing novel treatments

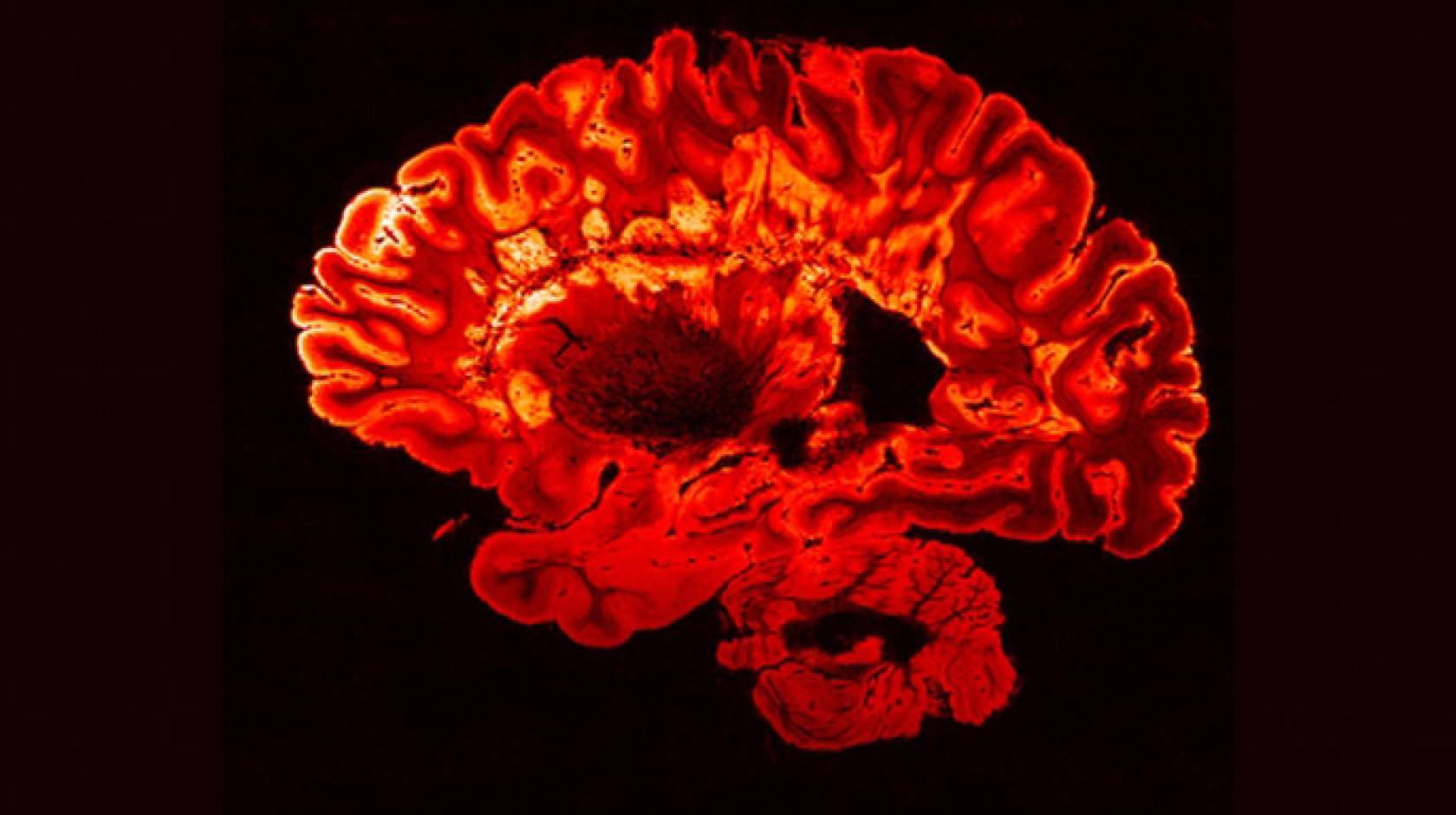
Credit: Steve Babuljak
Canada and the U.S. have among the highest rates of MS in the world, with around three in every thousand individuals affected. Symptoms can include fatigue, poor coordination, tingling, organ problems and cognitive impairment. There is no cure, although quicker diagnoses and better drugs have improved outcomes significantly in the last 15 years.
“IgAs comprise 80 per cent of all antibodies in the body, yet their exact function is still not fully understood,” said Sergio Baranzini, Ph.D., a co-author on the paper who is a professor of neurology in the UCSF Weill Institute for Neurosciences. “Showing that IgA-producing B cells can travel from the gut to the brain opens a new page in the book of neuroinflammatory diseases and could be the first step towards producing novel treatments to modulate or stop MS and related neurological disorders.”
The lead authors on the work are postdoctoral fellows Olga Rojas, Ph.D., and Elisa Porfilio, Ph.D., from the Gommerman lab at the University of Toronto and Anne-Katrin Pröbstel, M.D., from the Baranzini lab at UCSF. In a moment of scientific serendipity, they recently presented their research at the same conference and realized their results aligned. The researchers began to collaborate, and Pröbstel and colleagues in the Baranzini lab were able to show that the Gommerman lab’s findings in mice had parallels to human MS patients.
Specifically, the UCSF team found evidence that IgA was decreased in fecal samples from patients with active MS neuroinflammation, suggesting that the inflammation-suppressing cells had been recruited to help fight the patients’ disease.
‘There is something very critical about how the gut and brain are connected’

Credit: Sherman Jia
One promising aspect of the new research is that increasing the number of IgA plasma cells that migrate from the gut to the brain eradicated neuroinflammation in mice. A therapeutic approach might aim to expand the number of these cells in the gut, enabling a plentiful supply that could move to the brain and dampen inflammation.
“As a clinician-scientist, it is exciting that our experiments linking preclinical animal models to the biology we see in real MS patients may have uncovered a general mechanism for how the immune system counteracts inflammation,” said UCSF’s Pröbstel. “Until now, no one has really studied these IgA-producing plasma cells in the context of disease, but we are now examining them in detail in patients with MS to begin to understand how we might manipulate them to help treat neuroinflammatory disease.”
A key next step for the researchers is to figure out what microbes in the gut promote the generation of immunosuppressive IgA plasma cells. “If we can understand what these cells are reacting to, we can potentially treat MS by modulating our gut commensals,” said Gommerman, referring to the bacteria that live in the healthy gut. “That might be easier than getting drugs into the brain, which is a strategy that hasn’t always worked in MS.”
The study also raises questions about the microbiome and lifestyle choices. Do certain lifestyles nudge some people toward a gut microbiome that allows immunosuppressive plasma cells to flourish? Are specific foods conducive to creating that environment and if so, might a drug or supplement mimic the effect? Genetics are just one factor that affect susceptibility to MS; the current study highlights how non-genetic factors may confer disease resistance.
Gommerman plans to pursue the basic science behind these questions, working with Baranzini and other research groups to bring the findings into the clinical realm. “There is something very critical about how the gut and brain are connected, and we’re starting to unravel the molecular threads behind that clinical observation,” she said. “It’s a great example of how fast science can move.”