Nicholas Weiler, UCSF

When given access to alcohol, over time mice develop a pattern similar to what we would call “problem drinking” in people, but the brain mechanisms that drive this shift have been unclear. Now a team of UC San Francisco researchers has identified a protein that links alcohol consumption with structural changes in one of the “reward centers” in the mouse brain.
The work, published online Sept. 7, 2017, in Neuron, casts new light on the molecular domino effect by which alcohol triggers long-lasting changes in brain cells that drive heavy drinking, the scientists said.
Though it is legal and easily obtained, alcohol remains an unusual and mysterious drug on a scientific level. Researchers still don’t know how ethanol — a tiny molecule that, unlike all other drugs of abuse, does not have a specific site of action — can alter brain function to promote compulsive, uncontrolled consumption and alcohol-seeking despite negative consequences.
“There is — rightfully — a lot of media attention right now on opiate abuse and addiction,” said Dorit Ron, professor and Endowed Chair in Cell Biology of Addiction in UCSF’s Department of Neurology, and the new study’s senior author. “But alcohol abuse and addiction are much bigger problems, and the human cost is staggering: 3.3 million people die every year in the world from alcohol abuse. Unfortunately, there are only a few medications on the market to reduce craving and relapse, and none of them work very well.”

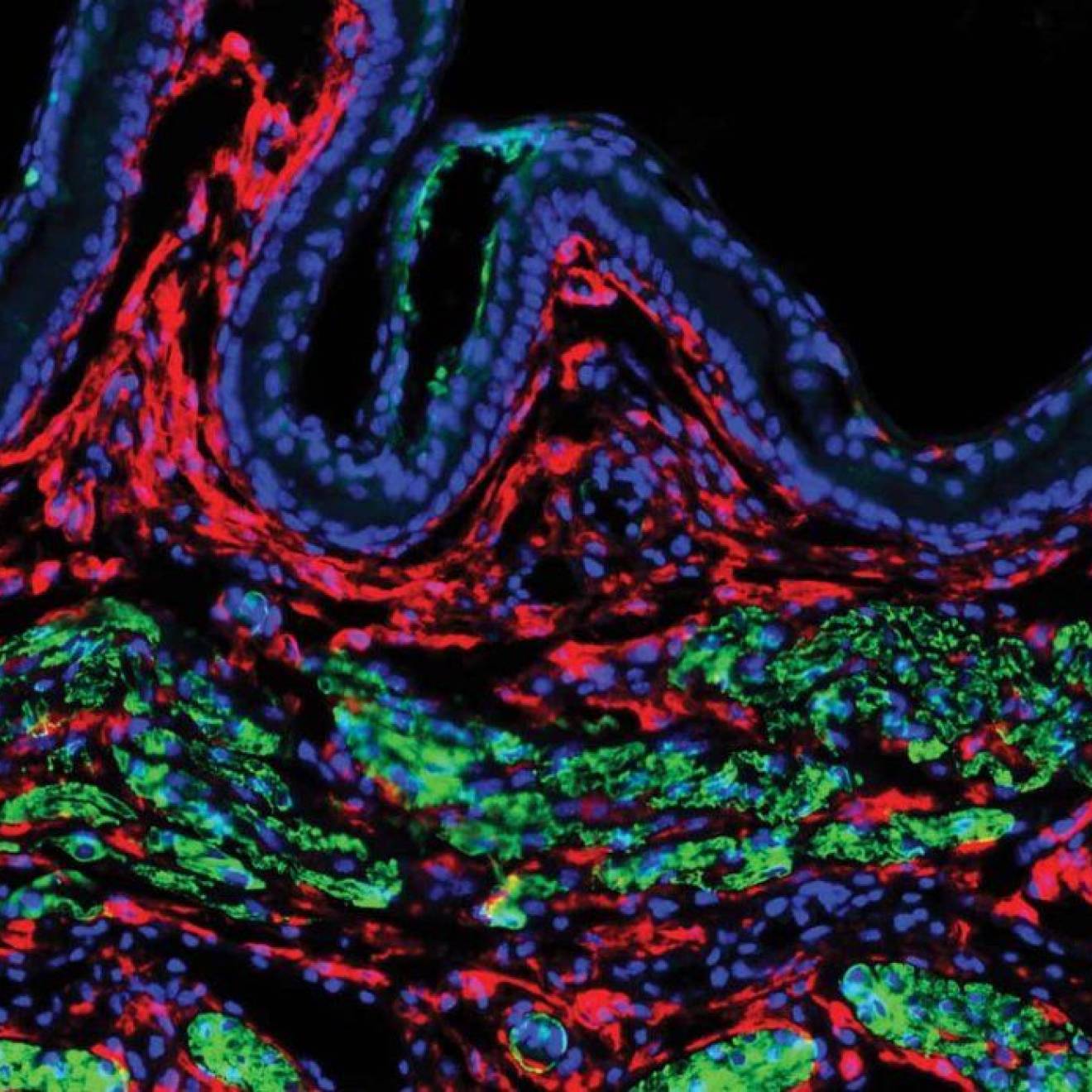
Credit: UCSF
Previous work in rodents by the Ron lab and others has suggested that a protein by the name of mTORC1 may be a key mediator of addiction to multiple drugs of abuse, including cocaine, morphine and alcohol. In earlier studies, her lab has shown that excessive drinking boosts mTORC1 activity in the nucleus accumbens, an important part of the brain’s reward circuitry, and that this increased mTORC1 activity is associated with alcohol-seeking. These findings suggested that mTORC1 might trigger structural changes in the nucleus accumbens that reinforce positive associations with alcohol, contributing to the cycle of excess drinking.
Earlier work from Ron’s lab also found that blocking mTORC1 activity with rapamycin, a common immunity-suppressing drug, caused rodents to significantly cut down their drinking — without impacting their taste for other rewarding substances, such as sugar water. But because rapamycin has significant side effects, it is unsuitable to treat people with alcohol use disorder. In order to help in the search for new, more specific drugs to treat alcohol abuse, Ron’s team wanted to better understand mTORC1’s role in alcohol addiction.
mTORC1’s normal function is to promote the synthesis of new proteins, so in the new study, postdoctoral associate Sophie Laguesse and her colleagues in the Ron lab used a technique called RNAseq to hunt new proteins that might be linked to mTORC1 activity in the mouse brain in response to alcohol.
Of the 12 proteins they found, the researchers focused on one called prosapip1 — an earlier study had shown that it plays some role at synapses, although its specific function had not yet been identified. They found that that this protein changes the structure and activity of neurons in the nucleus accumbens after mice drank alcohol for a long time. When the authors genetically blocked the production of prosapip1, these alcohol-dependent changes were significantly reduced, and when offered a choice between alcohol and water, mice in which prosapip1 was blocked reduced their preference for alcohol.
This reduction in alcohol preference was quite specific: the mice’s consumption of sugar water, normally very rewarding, was not affected by blocking the protein.
“We have identified a new protein that plays a crucial role in changing the landscape of neurons in the nucleus accumbens, which then leads to escalation of problem drinking,” Ron said. “These findings open up research into the protein’s role in neural plasticity, and also into how alcohol and other drugs of abuse alter our brains.”
The findings plant mTORC1 and associated molecules firmly into neural pathways that allow drug abuse, and Ron hopes that future research will allow scientists to develop new, highly targeted approaches to treating the widespread scourge of addiction.
“I’ve been doing research on the molecular neurobiology of alcohol abuse for many years and this is the first time I’ve seen a signaling molecule that appears to be shared by many drugs of abuse,” Ron said. “I think in a way this may be a gateway to understanding drug addiction — it’s a very exciting time.”
The research was supported by National Institute of Alcohol Abuse and Alcoholism (NIAAA) grants P50AA017072, P50AA010761, and ZIA-AA000421 and the Belgian American Educational Foundation.
Additional authors on the paper were Nadege Morisot, Feng Liu, Samuel A. Sakhai, Khanhky Phamluong and Kevin J. Bender of UCSF; Jung Hoon Shin, Martin F. Adrover and Veronica A. Alvarez of the NIAAA; and Marcelo F. Lopez, William C. Griffin III and Howard C. Becker of the Medical University of South Carolina.