Ashley Fong, UC Irvine via The Conversation
Heart disease is the No. 1 cause of death in the US. The most common type is coronary heart disease, which occurs when there’s a buildup of plaque within the heart’s blood vessels. Smoking, diabetes, obesity and high blood pressure all can contribute. When there’s a complete blockage — a heart attack — a large portion of the heart muscle dies. The heart responds by creating scar tissue, eventually leading to heart failure — the heart muscle just can’t pump enough blood to the rest of the body.
Credit: NIH: National Heart, Lung and Blood Institute
Currently, the only treatment options for damaged heart muscle are surgery, if possible, and for the worst cases, a whole heart transplantation. But there’s a huge shortage of organs for transplantation, and for this reason, we need to find new strategies to treat heart disease.
Stem cells have great potential to fill this void. They’re a unique type of cell that starts out unspecialized but can multiply and turn into specialized cells of the adult body – for instance, brain cells or heart muscle cells, officially called cardiomyocytes.

Credit: Ashley Fong, CC BY-ND
Stem cells may be useful in tissue engineering therapies; researchers build tissues from them in the lab to transplant and replace damaged muscle. They could potentially be used in cellular therapies; researchers inject the heart cells into the heart and allow for regeneration. Right now, one ongoing clinical trial injects a heart attack patient’s own heart stem cells back into the patient’s heart to decrease scar size and promote heart regeneration. In addition, stem cells can also be used as a drug-screening platform in order to find new drugs to treat heart disease.
These options rely on turning stem cells into heart muscle cells – but even once they differentiate, the heart cells remain immature. They’re not fully developed, having characteristics you’d find in a fetus, not an adult. To advance these possible therapies, we need ways to take these heart muscle cells one step further, to maturity. I’m studying how the heart’s natural environment affects that maturation process. I focus on how the extracellular matrix, or scaffold, of the heart affects maturation. The overall goal is to find a way to create from stem cells fully functioning, mature heart cells that can be safely and effectively used for transplantation therapies and drug screening applications.
Adult cells to stem cells to immature heart cells
There are many kinds of naturally occurring stem cells, but I work with a type that can be made from the adult body. For example, I can take your regular skin cell or blood cell and transform it in the lab into a stem cell by using viruses to introduce stem cell genes into it. The official name for what I wind up with after three or four weeks is “induced pluripotent stem cells.”
This new stem cell has the unique ability to replicate and turn into almost any cell of the adult body. Since they can be made from a patient’s own cells, the induced pluripotent stem cells retain the patient’s specific genetic information. That’s a big benefit when transplanting the cells – there’s no need for immunosuppression to avoid rejection of the new tissue by the patient’s body. It also allows a patient’s specific disease to be modeled in the lab, in hopes of finding a customized drug or therapy for this individual’s particular disease. This situation is sometimes called a “clinical trial in a dish.”
Credit: Kimberly Lim, CC BY-ND
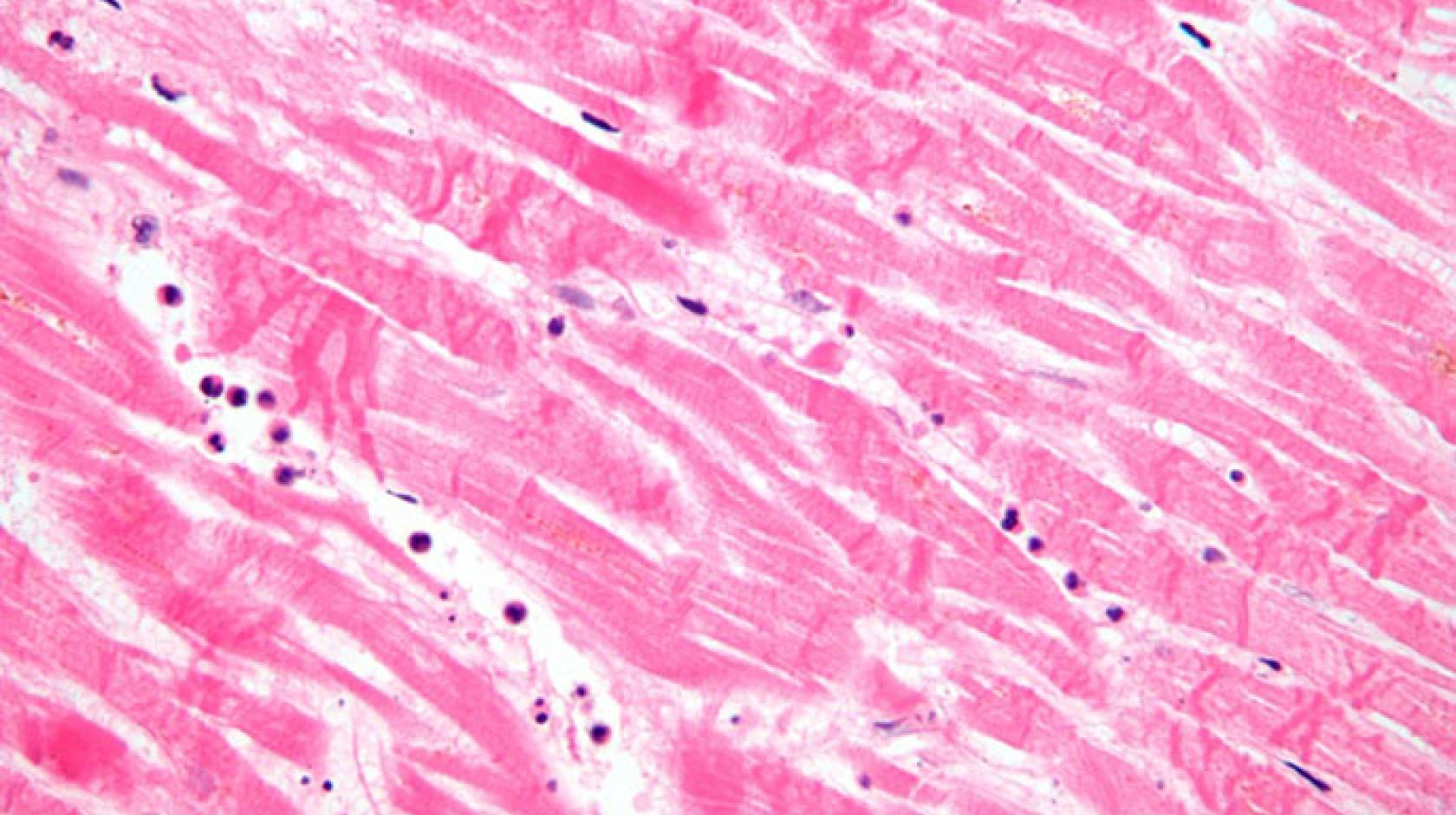
After years of hard work, I was finally successful at manipulating the stem cells into heart muscle cells in the lab. I had to find the perfect stem cell line and protocol to use, which required lots of trial and error. It was very exciting to finally see the beating heart muscle cells in my petri dish!
But the cells' ability to beat on their own actually demonstrates that they’re immature, and thus shouldn’t be used in treatment and drug screening. They spontaneously beat inappropriately. They don’t have the proper machinery to contract with the necessary force. These actions could have dangerous consequences if we were to rely on immature cells in a patient’s heart. Mature cardiomyocytes beat in response to a signal from the heart’s pacemaker cells, avoiding the safety risk of arrhythmia. And mature cells are strong enough to pump blood throughout the body.
So I need to figure out how to mature these cells.
Scaffold provides more than just structure
Within heart tissue, a scaffold surrounds the cells and provides structural support. The tissue is like a brick wall; the bricks are the cells and the mortar is the scaffold of proteins that holds everything together. Just as crucially, in a healthy heart, the scaffold sends signals to the heart cells to behave a specific way that allows them to survive and function normally.
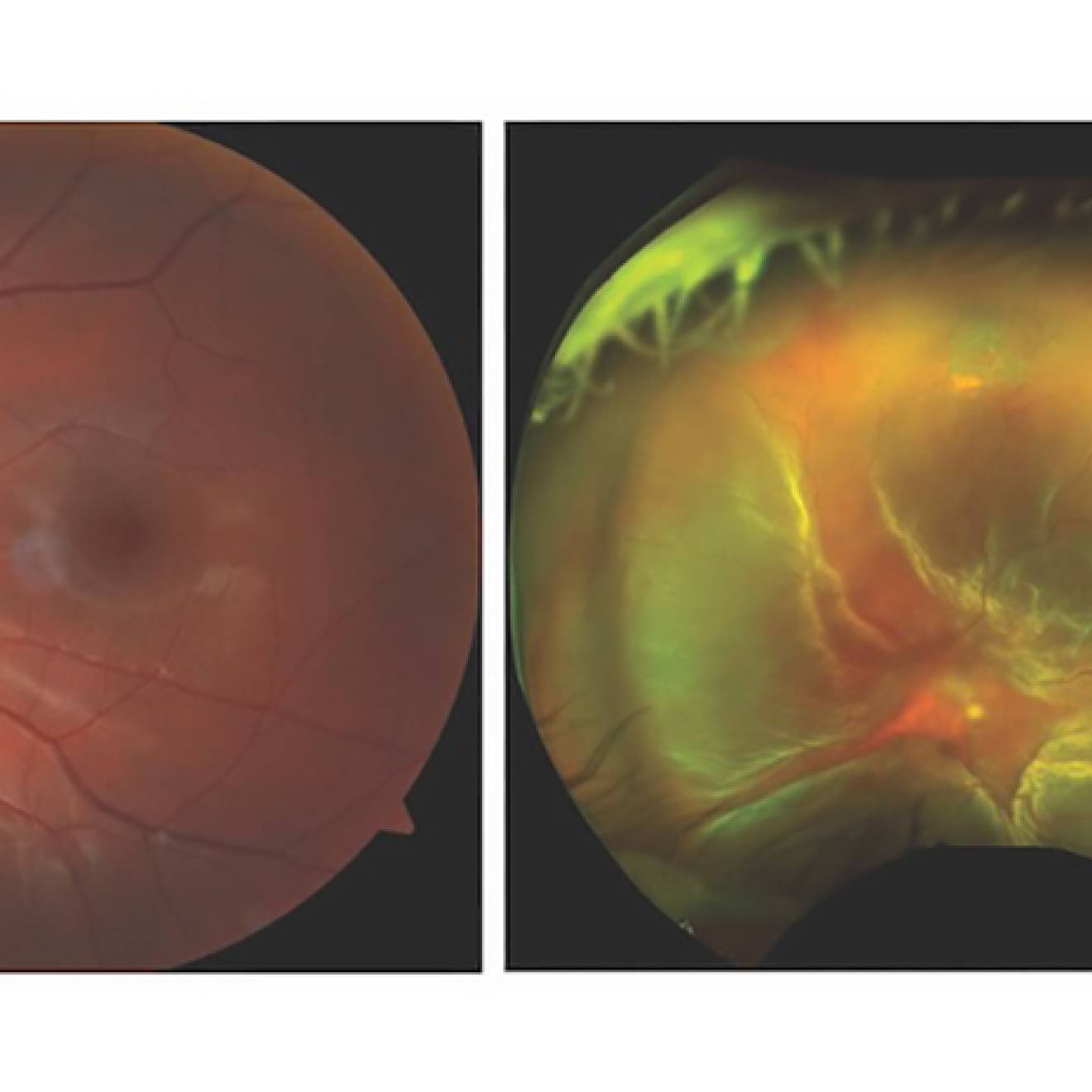
Credit: Ashley Fong, CC BY-ND
I obtain the heart scaffold by extracting it from cow hearts. I use detergents to remove the heart cells, similar to how laundry detergent removes dirt from clothes. Once all the cells are removed, only the scaffold remains. It’s made up of a network of fibers consisting of collagen, fibrinogen, elastin and other types of extracellular matrix proteins. After a few more steps, I get the scaffold into the form of a 3D gel – now it has a texture similar to Jello, which I can shape.
When I put my human stem cell-derived heart muscle cell into the adult heart scaffold, it matures. The process works by increasing the amount of some important proteins, including those that handle calcium. That improves calcium signaling, which is essential for the cell to contract.
Credit: Ashley Fong, CC BY-ND
I also discovered that the most maturation occurs when the cells are grown in a 3D scaffold, rather than a 2D scaffold in a traditional flat petri dish. This finding supports the idea that placing the cells in an environment more like their natural habitat can instruct them to develop and mature. We still don’t know how the scaffold actually issues its instructions to the cardiomyocytes to mature, but for now we’re glad it seems to work.

Credit: Ashley Fong, CC BY-ND
We’re another step closer to being able to use mature stem cell-derived cardiomyocytes in new advanced treatment options to cure heart disease. I’m working on just a small sliver of the type of research that’s needed to get stem cells ready to be used to treat diseases. Stem cell research gives patients and their families hope, but cures won’t happen overnight. Even when we’re not seeing immediate results, stem cell research needs continued support so we researchers can develop the cures we so desperately need.
Ashley Fong, Ph.D. student in molecular biology & biochemistry, University of California, Irvine
This article was originally published on The Conversation. Read the original article.