Nina Bai, UCSF

Wildfires are again raging in California, but this year’s season began in a perfect storm of smoke from the blazes, a scorching heat wave, and the ongoing COVID-19 pandemic.
During a typical wildfire season, hospitals see more people coming in for respiratory issues, said Stephanie Christenson, M.D., assistant professor of pulmonology at UC San Francisco. The worry this year is that the smoke from wildfires could increase the severity of COVID-19 symptoms.
Though there have yet to be studies looking specifically at the effect of wildfire smoke on COVID-19, there is preliminary research linking air pollution to increased COVID-19 susceptibility, severity and death, said Christenson.
With wildfire smoke, and air pollution generally, the most concerning are the microscopic particles that are about 2.5 microns in size (about 30 times smaller than the width of a human hair), which can be inhaled deep into the lungs, said John Balmes, M.D., professor of medicine. There, these tiny toxins can injure the lining of the lungs, in a process known as oxidative stress, and cause airway inflammation.
Added injury to the lungs
People with certain chronic respiratory conditions, such as asthma, already have airway inflammation, and the added inflammation from wildfire smoke would be particularly harmful, said Balmes. “There is no question that wildfire smoke can exacerbate these pre-existing conditions.”
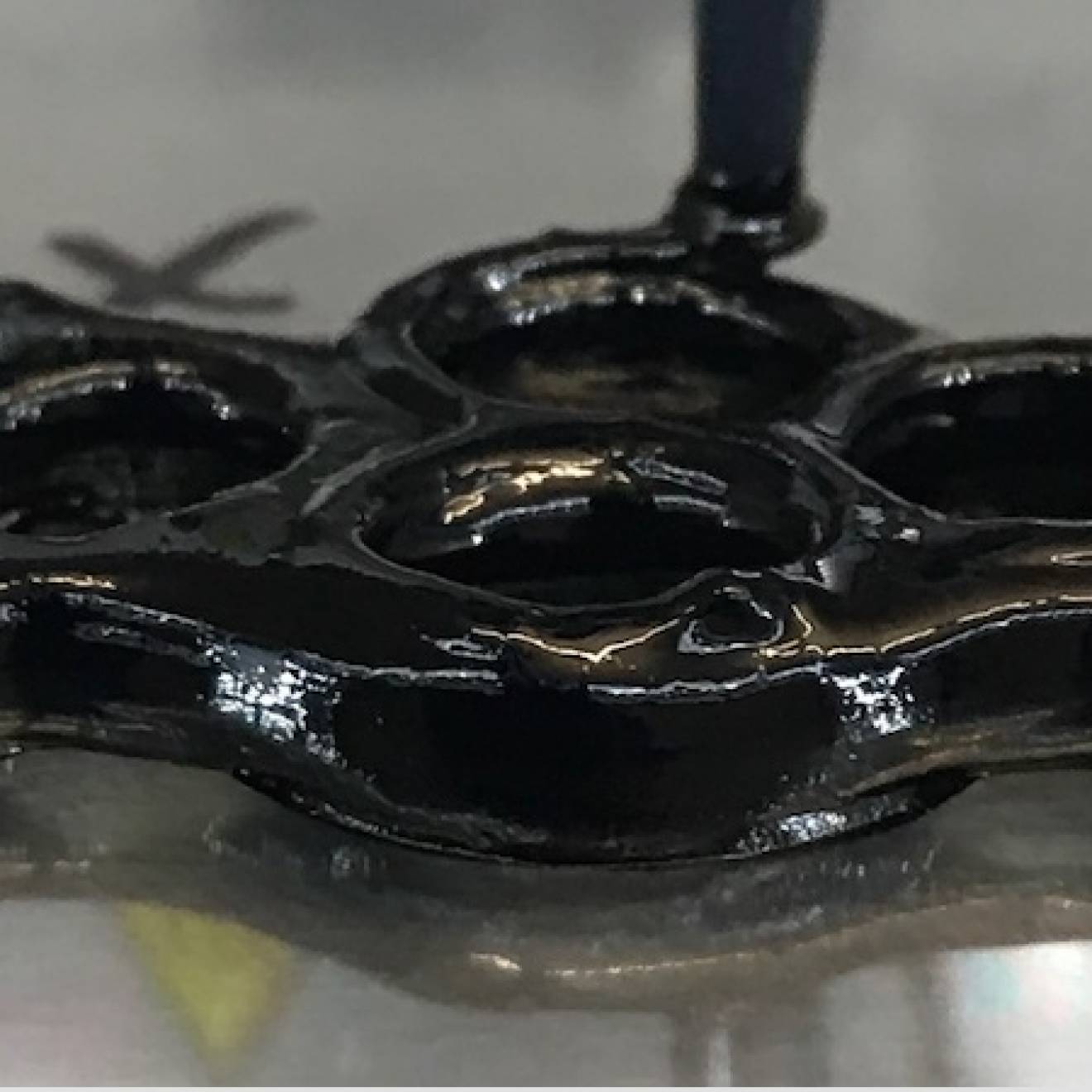
Research also has shown that wildfire smoke raises the risk of lower respiratory tract infections such as acute bronchitis and pneumonia, by impairing the immune response, said Balmes. The immune cells, known as alveolar macrophages, that patrol our lower lungs are adept at engulfing and digesting foreign particles, such as bacteria. But when these macrophages engulf the combustion particles in wildfire smoke, they cannot digest them, and essentially are disabled from performing their role in the immune response.
Wildfire smoke, like COVID-19, can affect more than the lungs. A study from the 2015 wildfire season found that emergency room visits in areas most affected by smoke increased not only for respiratory complaints, but also cardiovascular and neurological complaints, such as stroke, said Jahan Fahimi, M.D., Ph.D., an emergency care physician.
Best to stay home
“My advice to the public is that people should be sheltering in place as much as possible,” said Balmes. “Stay home with windows closed, ventilation turned to recirculate, and if possible, have a clean air room with a HEPA air purifying appliance.”
To avoid COVID-19 exposure, it’s safest to stay home with the people you already live with, added Fahimi.
As for masks, Balmes noted that N95 masks fitted tightly over the face offer the best protection against wildfire smoke particles, but that N95 masks with exhalation valves do not provide COVID-19 protection. He recommends covering the valve with tape or wearing a surgical mask over the N95.
Because N95 masks (without valves) should be reserved for health care workers treating COVID-19, experts do not suggest buying new N95 masks unless you need to be outside for an extended period of time.
Duration of smoke exposure determines risk
Fahimi drew a parallel between wildfire smoke and the coronavirus — that in both cases, the duration and dose of exposure determines risk. “If you’re only going to be out for 10 to 15 minutes, even no mask is fine for a short duration,” he said. “But people working outdoors, that’s when you want a mask.”
Surgical masks are more readily available and will provide some protection against wildfire smoke, said Balmes. Cloth masks likely provide little protection against PM2.5 particles, but are still essential for COVID-19 protection.
“If you can’t get a surgical or a N95 mask, wear a cloth mask because the most important thing is to protect others from the virus,” said Balmes.