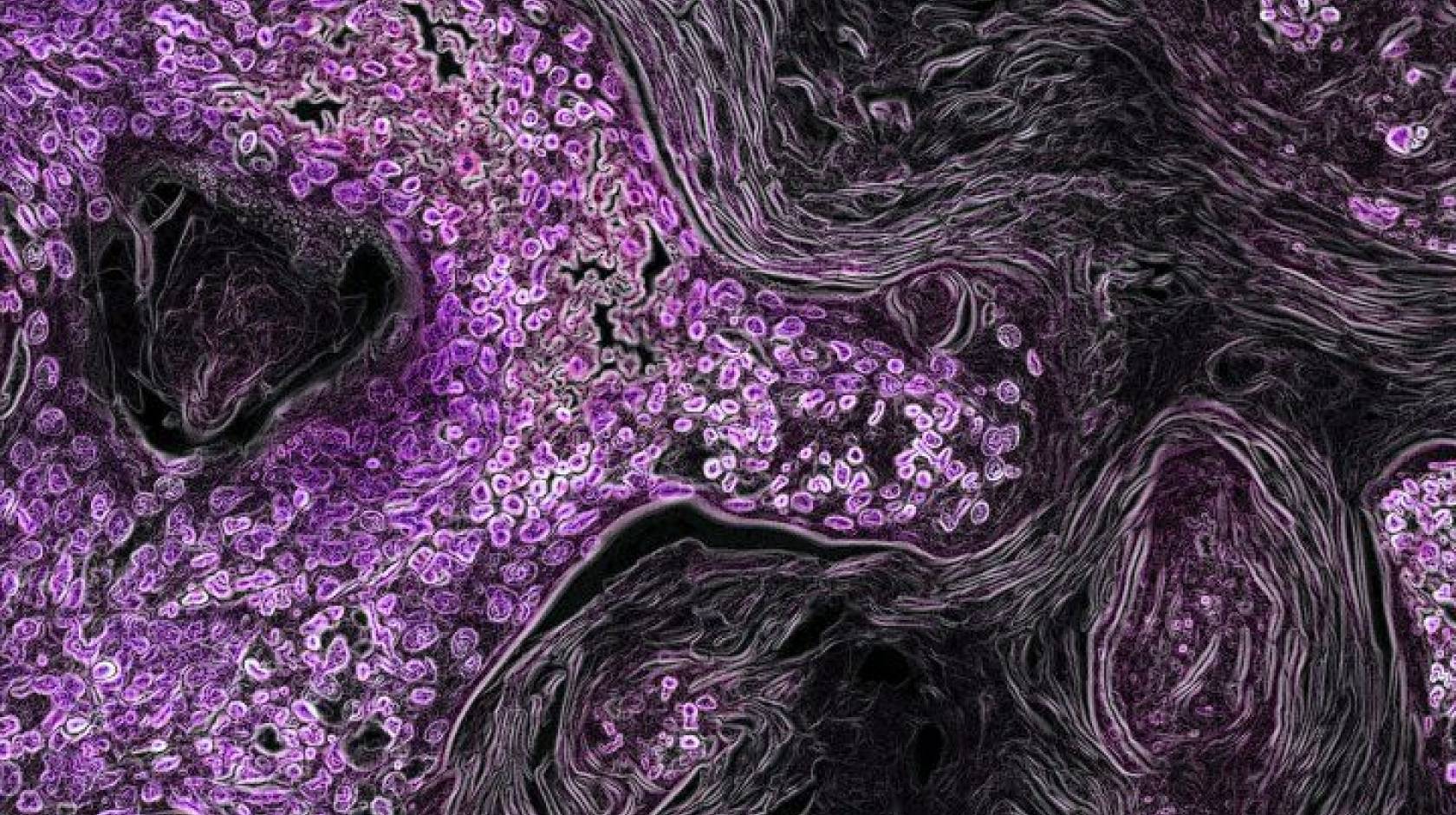
Robin Marks, UCSF
Researchers at UC San Francisco have successfully leveraged an FDA-approved drug to halt growth of tumors driven by mutations in the RAS gene, which are famously difficult to treat and account for about one in four cancer deaths.
Taking advantage of what they discovered to be the cancer cells’ appetite for a reactive form of iron, the researchers tweaked an anticancer drug to operate only in these iron-rich cells, leaving other cells to function normally. The achievement, described in the March 9 issue of the Journal of Experimental Medicine, could open doors to more tolerable chemotherapy for many cancers in which current treatments can be as challenging as the disease.
“RAS mutations, by themselves, cause more misery than all other cancers combined, and take so many lives worldwide,” said Eric Collisson, M.D., a senior author of the study and member of the UCSF Helen Diller Family Comprehensive Cancer Center. “This study brings us much closer to addressing the unmet need for better treatment of these cancers.”
A cancer drug with an iron sensor
To do so, Collisson and lead author Honglin Jiang, M.D., both oncologists at UCSF, teamed up with Adam Renslo, Ph.D., a pharmaceutical chemist also at UCSF and co-senior author, to focus on RAS-mutated pancreatic and gastrointestinal cancers. The RAS gene plays a role in tamping down pathways in the cell that drive it to grow and divide. Mutations in the gene usually mean that these growth forces are going unchecked, leading to cancer.
Current treatments, such as a drug called cobimetinib, do a good job of blocking this excessive growth activity set in motion by the mutation, but they do so in many other, non-cancerous tissues as well, leading to serious side effects that many patients find intolerable.
“Cobimetinib is a classic example of an anticancer drug that we know works well on its target, but it hasn’t achieved its clinical potential because the same target is important in the skin and other normal tissues,” said Renslo.
The researchers found that many tumors driven by the KRAS form of RAS mutations have elevated concentrations of ferrous iron — a form of the element that is highly reactive — and that this is correlated with shorter survival times.
To take advantage of this unique characteristic of the cancer cells, Renslo and then-graduate student Ryan Muir synthesized a new version of cobimetinib bearing a small, molecular sensor of ferrous iron. The sensor effectively turns cobimetinib off until it encounters ferrous iron in the cancer cells.
After confirming that the new drug, dubbed TRX-cobimetinib, prevented adverse effects on normal tissues like skin that limit dosing in human patients, the researchers tested the compound in mouse models of several KRAS-driven cancers and found that it was just as effective as cobimetinib in shrinking tumors.
Enabling new drug combinations
The reduced toxicity allowed the researchers to combine TRX-cobimetinib with other synergistic anticancer drugs to provide combination treatments that proved even better at inhibiting tumor growth and were better tolerated than comparable combinations using cobimetinib.
“By removing toxicity from the equation, you’re talking not just about one new drug, but 10 new combinations that you can now think about exploring in the clinic,” said Renslo. “That would be the home run for this approach.”
Renslo is already at work studying whether a similar approach can be applied to antibiotics, some of which have untoward side effects, to target treatment and reduce toxicity.
Collisson, who works every day with patients wrestling with these cancers, said the collaboration with Renslo has given him hope that he’ll be able to give those patients better options in the not-too-distant future. And, he added, the experience has opened his eyes to things he’d been missing by being so focused on his day-to-day oncology world.
“I love taking care of patients, and a fundamental part of that is, ultimately, getting a molecule to the place where it’s needed and keeping it out of places where it’s not needed,” he said. “To be able to deliver a therapy that’s five times more potent than what we currently have and not run the patient ragged, that’s pretty exciting.”
Authors: Additional authors of the study are Ryan Gonciarz, Adam Olshen, Iwei Yeh, Byron Hann, Ning Zhao, Yung-hua Wang, Spencer Behr, and Michael Evans, all of UCSF; and James Korkola, of Oregon Health & Sciences University.
Funding: This work was supported by NIH, NCI Grants CA178015, CA222862, CA227807, CA239604, CA230263, CA210974, CA224081, P30CA082103, AI105106, W81XWH1810763, and W81XWH1810754. See the study for additional funding.

